We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Left ventricular assist device
From WikEM
(Redirected from LVAD)
Contents
Background
- Commonly referred to as an LVAD
- Developed in 1960s and used as a bridge to Cardiac Transplant but have evolved into permanent, or “destination therapy"
- Indication is New York Heart Association class 4 heart failure, ejection fraction <25%, VO2 max less than 15 among other criteria[1]
- Goal of a VAD is to assist the ventricle and augment cardiac output
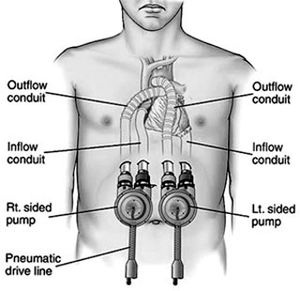
- LVAD (left ventricle), RVAD (right ventricle), BiVAD (both venticles via separate pumps)[2]
- VADs have 3 major variables:
- Speed
- Flow
- Power
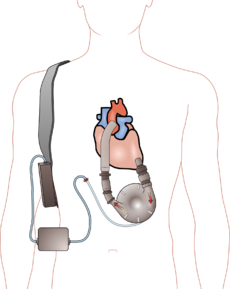
Components
- Pump = Internal pump (usually placed in preperitoneal space), takes blood from a cannula in the apex of the left ventricle and pumps it into the aorta
- Driveline = Percutaneous cable that exits the abdominal wall, connects pump to external components (controller, battery)
- Controller = External "box" containing computer for the device that monitors pump performance, has a display screen and controls for settings/alarms/diagnostics, and will display will show pump speed in RPM and pump output in L/min
- Power Supply = Controller can be connected to batteries for patient mobility, or to a "power base station" that plugs into the wall for home use
Devices Overview
HeartMate I or XVE
- Use: Destination Therapy
- Flow Type: Pulsatile
- Backup Method: Hand Pump
- Battery: 12volt MiMH - 10hrs
- Defib/Cardioversion: Use hand pump during defib/cardioversion
HeartMate II
(Most common type in use today)
- Use: Bridge to transplant or destination therapy
- Flow type: Continuous
- Backup Method: No external method
- Battery: 14V Li-Ion - 10 hrs
- Defib/Cardioversion: No precautions
Thoratec VAD (HeartMate III)
- Use: Bridge to Transplant
- Flow Type: Pulsatile
- Backup Method: No external method
- Battery: 12V lead acid gel battery - 7.2 Ah - up to 3 hrs
- Defib/Cardioversion: No precautions
Complications/Differential Diagnosis[3]
- Bleeding - most common reason for ED visit (frequency 42%[4])
- GI Bleed, epistaxis, ICH, intrathoracic bleeding
- Mechanisms:
- acquired Von Willebrand Disease (vWD)
- supratherapeutic anticoagulation
- lack of pulsatile flow → AV malformations in GI tract
- Immediately consult VAD team/coordinator
- treatment - anticoagulant reversal based on specific agents used
- In life-threatening bleeds, consider TXA, PCC, Desmopressin, FFP
- Warfarin reversal carries low risk for acute thrombosis [5]
- Infection - driveline and pocket are most common sites[4]
- Usually gram positive bacteria, but also need to cover for fungal infection
- Pump Thrombosis
- Low output state with falsely elevated pump flow estimates on controller
- Diagnose with echo or cardiac CTA
- treatment with heparin and antiplatelet therapy
- Consider tPA in severe (life-threatening) situations
- Arrhythmia - very common
- Get labs to evaluate electrolytes and troponin
- treatment atrial fibrillation as in any other patient
- treatment ventricular arrhythmias with volume replacement and pharmacological or electrical cardioversion
- Place pads anterior/posterior if going to cardiovert/defibrillate
Evaluation[3]
- Assess perfusion and general state (mental status, skin temp/color, capillary refill, etc)
- LVADs are preload dependant - if symptoms of hypoperfusion, give fluid blous
- HR measured via ECG or auscultation (may be difficult secondary to pump noise)
- Get 12-lead ECG on all LVAD patients
- Demonstrates primary cardiac disease[6]
- Generally, VAD does not influence underlying cardiac rhythm
- Blood pressure measured with manual BP cuff and Doppler ultrasound - MAP is identified when constant flow is heard
- MAP should be 70-90 mmHg
- Can also monitor with arterial line
- Basic labs (CBC, CMP, Coags) should be obtained on all LVAD patients
- Assess LVAD status
- Auscultate for pump noise
- Device parameters (found on controller)
- Pump speed - varies by device - 2,000-10,000 RPM
- Power - normal 4-6 Watts
- Flow - normal 4-6 L/min
- Pulsatility Index (PI) - normal 1-10
- Measures magnitude of pulsatile flow provided by native cardiac contractions
- Higher PI = less LVAD support
- Clinical status more important than LVAD parameters
Management
- Immediately contact hospital or patient's LVAD coordinator to help coordinate care
- Take special care to not twist, bend, cut, or otherwise damage the driveline
- First generation LVADs had pulsatile flow
- Subsequent designs use continuous flow - patient will not have a palpable pulse
- Patient will be on anticoagulation and antiplatelet therapy secondary to high risk of pump thrombus, CVA, and other thromboembolic events
- VADs are ECG independant, unlike ICD (many patients with a VAD will also have an ICD in place)
- ICD discharges are common, and frequently inappropriate (possibly secondary to LVAD interference)[6]
Cardiac Arrest[3]
- Unconscious, apneic, no evidence of LVAD function (auscultate for mechanical noise)
- Immediately evaluate LVAD components and attach to reliable power source
- Some first-generation LVADs have external hand pumps that can be used to provide circulation
- Otherwise follow ACLS as in a normal patient
- Patient should be intubated, given IV fluids and drugs, etc
- Avoid chest compressions unless absolutely necessary - evaluate other causes of pump failure or lack of perfusion (e.g. pump thrombus) first
- Compressions can potentially damage LVAD, disrupt its connection to the heart (risk of exsanguination), etc
- Some studies available[7][8] indicate that CPR may not be as harmful as currently thought, or that abdominal compressions are an alternative[9] but further investigation needed
- Use clinical judgement for initiation of compressions
Disposition
- Immediately contact the patient's VAD coordinator
- Almost all LVAD patient presenting to the ED will require admission
See Also
External Links
References
- ↑ Mancini D, Lietz K. Selection of cardiac transplantation candidates in 2010. Circulation. 2010;122(2):173-83.
- ↑ Mechem CC. Prehospital assessment and management of patients with ventricular-assist devices. Prehosp Emerg Care. 2013 Apr-Jun;17(2):223-9.
- ↑ 3.0 3.1 3.2 Partyka C, Taylor B. Review article: ventricular assist devices in the emergency department. Emerg Med Australas. 2014 Apr;26(2):104-12.
- ↑ 4.0 4.1 Rose EA, Gelijns AC, Moskowitz AJ et al. Long-term use of a left ventricular assist device for end-stage heart failure. N. Engl. J. Med. 2001; 345: 1435–1443.
- ↑ Jennings, D, et al. Safety of Anticoagulation Reversal in Patients Supported with Continuous-Flow Left Ventricular Assist Devices. ASAIO Journal. July 2014. 60:381–384
- ↑ 6.0 6.1 Pistono M, Corrà U, Gnemmi M, Imparato A, Temporelli PL, Tarro Genta F, Giannuzzi P. How to face emergencies in heart failure patients with ventricular assist device. Int J Cardiol. 2013 Oct 15;168(6):5143-8
- ↑ Shinar Z, Bellezzo J, Stahovich M, Cheskes S, Chillcott S, Dembitsky W. Chest compressions may be safe in arresting patients with left ventricular assist devices (LVADs). Resuscitation. 2014 May;85(5):702-4.
- ↑ Mabvuure NT, Rodrigues JN. External cardiac compression during cardiopulmonary resuscitation of patients with left ventricular assist devices. Interact Cardiovasc Thorac Surg. 2014 Aug;19(2):286-9.
- ↑ Eric M Rottenberg, Jarrett Heard, Robert Hamlin, Benjamin C Sun, and Hamdy Awad. Abdominal only CPR during cardiac arrest for a patient with an LVAD during resternotomy: A case report. J Cardiothorac Surg. 2011; 6: 91.