We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Warfarin reversal
From WikEM
(Redirected from Warfarin (Coumadin) Reversal)
Contents
Background
- For supratheraputic INR on warfarin
- Intracranial hemorrhage is significantly increased with an INR > 4.0[1]
Target INR
- Vascular thrombosis (DVT, PE): 2.0-3.0
- Most mechanical heart valves: 3.0-4.5
- Bileaflet mechanical aortic heart valves: 2.5-3.5)
Risk Factors for INR > 6.0[2]
| Risk Factor | Odds Ratio |
| Malignancy | 16.4 |
| Tylenol Intake > 9100 mg/week | 10 |
| New Medication | 8.5 |
| Increased Warfarin Intake | 8.1 |
| Tylenol Intake 4550 mg - 9099 mg/week | 6.9 |
| Decrease Vitamin K intake | 3.6 |
| Acute Diarrheal Illness | 3.5 |
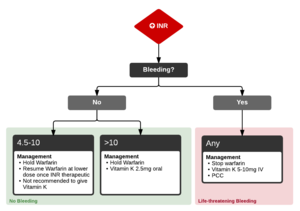
Treatment based on INR[3]
INR 4.5-10 No Bleeding
- Hold Warfarin
- Resume Warfarin at lower dose once INR therapeutic
- Not recommended to give Vitamin K
INR >10 No Bleeding
- Hold Warfarin
- Vitamin K 2.5mg oral
Major Bleeding
- Stop warfarin
- Give Vitamin K 5-10mg IV INR will decrease over 24-48 hours (small risk of anaphylaxis with IV Vitamin K)
- Give 4 Factor prothrombin complex concentrate (PCC)
- If no PCC, then give 15 ml/kg fresh frozen plasma (no benefit to combining PCC and FFP)
Consult cardiology in conjunction with hematology if patient has prosthetic valve
See Also
Video
References
- ↑ Hylek EM, Singer DE. Risk factors for intracranial hemorrhage in outpatients taking warfarin. Ann Intern Med.1994;120:897-902.
- ↑ Hylek, E et al. Acetaminophen and Other Risk Factors for Excessive Warfarin Anticoagulation. JAMA. 1998;279(9):657-662 PDF
- ↑ Holbrook A, et al; American College of Chest Physicians. Evidence-based management of anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141 PDF