Deadly Listeria Outbreak Halted in Record Time

Robert Tauxe, MD, MPH, deputy director of CDC's Division of Foodborne, Waterborne and Environmental Diseases
In 2011, cantaloupes contaminated with the bacteria Listeria monocytogenes caused the deadliest foodborne disease outbreak in the United States in nearly 90 years. The number of deaths would have been higher had it not been for an effective, coordinated response by the Centers for Disease Control and Prevention (CDC), state and local health departments, and the Food and Drug Administration (FDA). Lives were saved because the outbreak was detected, its source was identified, and a national warning was issued – all in just a matter of days.
"It's the fastest listeria investigation I’ve ever seen," said Robert Tauxe, MD, MPH, deputy director of CDC’s Division of Foodborne, Waterborne and Environmental Diseases, which works to prevent and control foodborne, waterborne, and fungal infections in the United States and globally.
Investment in Public Health Saves Lives
The September 2011 outbreak, which was linked to a single cantaloupe farm in Colorado, is a textbook example of how investments in coordinated public health response can save lives. Although the outbreak is tragic–killing 29 people and causing a miscarriage,* Dr. Tauxe estimates up to twice as many would have been infected had officials not had the tools, people, and systems in place that played a key role in the nationwide response. "By having rapid detection, rapid investigation, and rapid recall of the products, CDC and others could act fast," he said.
Listeria outbreaks are often difficult to investigate. The bacteria can stay in the body a long time before making a person sick, allowing more people to be infected by the same food source and leaving a cold trail for disease detectives trying to locate the outbreak’s origin. Listeria outbreaks can also be deadly, especially for the elderly, people with weak immune systems, developing fetuses, and newborn babies.
Yet during the recent listeria outbreak, only 10 days went by between when Colorado public health officials first spotted an unusual increase in listeria cases in local hospitals to identification of contaminated cantaloupes as the source, and a national warning of the danger was issued to consumers.
Below is a timeline of how medical and public health officials, CDC disease detectives, and regulatory officials worked together to stop the outbreak:
September 2-7 – Listeria 'spike' reported in Colorado
Local doctors report seven cases of listeria infection to the Colorado Department of Public Health and Environment – far more than usual – so public health officials start investigating. They contact patients for food history interviews, using a listeria questionnaire developed by CDC. In some cases, public health officials meet with relatives, as the patients with listeria infection have already died. In addition, the Colorado health department sends samples of listeria from patients to the Colorado public health laboratory for PulseNet “DNA fingerprinting”. PulseNet is a CDC network of public health laboratories that use a database to rapidly detect patterns in foodborne illnesses across the United States. "They track the individual ‘fingerprint’ pattern of bacteria, and when there’s a spike in numbers of one pattern, it raises a flag," Dr. Tauxe said.
September 6 – Multistate outbreak recognized
 Public health officials across the United States are alerted to the listeria strains identified in Colorado and CDC checks the PulseNet database for additional cases with these outbreak strains–identifying cases in 2 other states. "Everybody is looking for patterns all the time," Dr. Tauxe said. At this point in the investigation, the source of the outbreak is still a mystery. Disease detectives suspect several possibilities, including ham products and cantaloupe.
Public health officials across the United States are alerted to the listeria strains identified in Colorado and CDC checks the PulseNet database for additional cases with these outbreak strains–identifying cases in 2 other states. "Everybody is looking for patterns all the time," Dr. Tauxe said. At this point in the investigation, the source of the outbreak is still a mystery. Disease detectives suspect several possibilities, including ham products and cantaloupe.
September 9 – Cantaloupe determined to be source of listeria outbreak
Colorado public health officials learn from interviews with patients that all victims had recently eaten cantaloupe, with several naming a specific variety – Rocky Ford, a specialty cantaloupe prized for its sweetness. Health officials in other states are reaching the same conclusion from their patient interviews, while CDC is coordinating the multistate investigation.
Colorado immediately warns citizens to avoid eating cantaloupe. On the same day, the Colorado Department of Agriculture and the FDA start a trace back investigation to find the stores and then the producer that sold the contaminated cantaloupe.
September 10-11 – Contaminated cantaloupe traced to Colorado grower
Colorado Department of Agriculture and FDA officials narrow down the possible sources of the cantaloupes to several farms in Colorado. They visit the farms and collect cantaloupes for testing in the lab. In the end, Jensen Farms of Granada, Colorado, will be found to be the single source of the contaminated cantaloupe. When contacted by public health officials, Jensen Farms confirms that cantaloupes have already been shipped across the U.S.
"That's when we realized this could be nationwide," Dr. Tauxe said.
September 12 – CDC issues national listeria warning, saving many lives
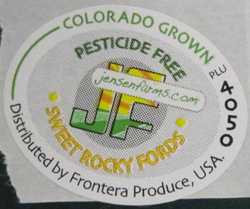 CDC, as administrator of the PulseNet lab network and the nationwide disease tracking sources, sends out a national warning to protect the health of all Americans from this listeria threat. CDC confirms three more cases have been identified outside of Colorado and warns all Americans at high risk of listeria infection not to eat cantaloupe sold as Rocky Ford-brand cantaloupe from Jensen Farms in Colorado.
CDC, as administrator of the PulseNet lab network and the nationwide disease tracking sources, sends out a national warning to protect the health of all Americans from this listeria threat. CDC confirms three more cases have been identified outside of Colorado and warns all Americans at high risk of listeria infection not to eat cantaloupe sold as Rocky Ford-brand cantaloupe from Jensen Farms in Colorado.
Two days later, the complete trace back and laboratory results from testing of cantaloupe confirm Jensen Farms as the outbreak source. All the cantaloupes are recalled and consumers are told to destroy any that they have not yet eaten. Another investigation is planned to determine how the cantaloupes came to be contaminated with listeria. Without PulseNet and the valuable work of many government agencies and health care professionals, Dr. Tauxe estimates up to 62 more people would have been infected by the cantaloupe, with up to 21 percent of those victims dying.
CDC Funding Critical to States' Ability to Respond to Foodborne Outbreaks
 In addition to epidemiological and laboratory expertise, CDC provides critical financial assistance to all 50 states, U.S. territories, and some local public health programs. This assistance gives states the ability to respond to major health threats – including foodborne disease outbreaks. CDC’s Epidemiology and Laboratory Capacity for Infectious Diseases Cooperative Agreement (ELC) provides states with essential laboratory and disease tracking funding, including a designated disease investigator and support for rapid laboratory testing.
In addition to epidemiological and laboratory expertise, CDC provides critical financial assistance to all 50 states, U.S. territories, and some local public health programs. This assistance gives states the ability to respond to major health threats – including foodborne disease outbreaks. CDC’s Epidemiology and Laboratory Capacity for Infectious Diseases Cooperative Agreement (ELC) provides states with essential laboratory and disease tracking funding, including a designated disease investigator and support for rapid laboratory testing.
Colorado was well-prepared to handle the listeria threat because of additional support from CDC. The state is one of only 10 states that are involved with FoodNet – a foodborne disease tracking network sponsored by CDC, FDA, and the U.S. Department of Agriculture. FoodNet provides additional support for states to track disease [3.4 MB] including additional staff. "More states should have this capacity, so that we can protect people everywhere from food outbreaks," said Dr. Tauxe.
*Reporting as of 0900 EDT on November 1, 2011.
- Page last reviewed: March 19, 2014
- Page last updated: March 19, 2014
- Content source:


 ShareCompartir
ShareCompartir