Mission Critical: Preventing Antibiotic Resistance
 Can you imagine a day when antibiotics don't work anymore? It's concerning to think that the antibiotics that we depend upon for everything from skin and ear infections to life-threatening bloodstream infections could no longer work. Unfortunately, the threat of untreatable infections is very real.
Can you imagine a day when antibiotics don't work anymore? It's concerning to think that the antibiotics that we depend upon for everything from skin and ear infections to life-threatening bloodstream infections could no longer work. Unfortunately, the threat of untreatable infections is very real.
Antibiotic resistance occurs when germs outsmart drugs. In today's healthcare and community settings, we are already seeing germs stronger than the drugs we have to treat them. This is an extremely scary situation for patients and healthcare workers alike.
So, what is fueling antibiotic resistance, you may ask? We're finding that the widespread overuse and incorrect prescribing practices are significant problems. In addition to driving drug resistance, these poor practices introduce unnecessary side effects, allergic reactions, and serious diarrheal infections caused by Clostridium difficile. These complications of antibiotic therapy can have serious outcomes, even death.
According to CDC's National Healthcare Safety Network, a growing number of healthcare-associated infections are caused by bacteria that are resistant to multiple antibiotics. These include: MRSA, vancomycin-resistant Enterococcus, extended-spectrum cephalosporin-resistant K. pneumonia (and K. oxytoca), E. coli and Enterobacter spp., carbapenem-resistant P. aeruginosa, carbapenem-resistant K. pneumonia (and K. oxytoca), E. coli, and Enterobacter spp.
So, what can we do to prevent antibiotic resistance in healthcare settings?
Patients, healthcare providers, healthcare facility administrators, and policy makers must work together to employ effective strategies for improving antibiotic use—ultimately improving medical care and saving lives.
Patients can:
- Ask if tests will be done to make sure the right antibiotic is prescribed.
- Take antibiotics exactly as the doctor prescribes. Do not skip doses. Complete the prescribed course of treatment, even when you start feeling better.
- Only take antibiotics prescribed for you; do not share or use leftover antibiotics. Antibiotics treat specific types of infections. Taking the wrong medicine may delay correct treatment and allow bacteria to multiply.
- Do not save antibiotics for the next illness. Discard any leftover medication once the prescribed course of treatment is completed.
- Do not ask for antibiotics when your doctor thinks you do not need them. Remember antibiotics have side effects.
- Prevent infections by practicing good hand hygiene and getting recommended vaccines.
Healthcare providers can:
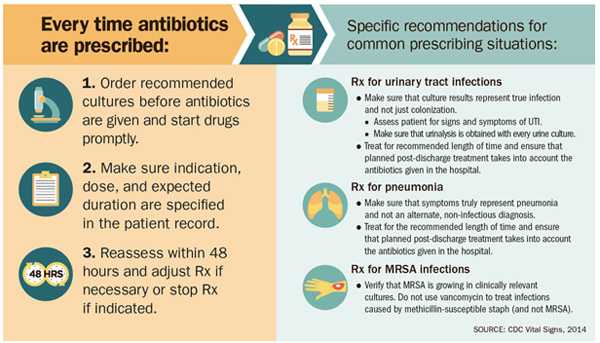
- Prescribe antibiotics correctly – get cultures, start the right drug promptly at the right dose for the right duration. Reassess the prescription within 48 hours based on tests and patient exam.
- Document the dose, duration and indication for every antibiotic prescription.
- Stay aware of antibiotic resistance patterns in your facility.
- Participate in and lead efforts within your hospital to improve prescribing practices.
- Follow hand hygiene and other infection control measures with every patient.
Healthcare Facility Administrators and Payers Can:
To protect patients and preserve the power of antibiotics, hospital CEOs/medical officers can:
- Adopt an antibiotic stewardship program that includes, at a minimum, this checklist:
- Leadership commitment: Dedicate necessary human, financial, and IT resources.
- Accountability: Appoint a single leader responsible for program outcomes. Physicians have proven successful in this role.
- Drug expertise: Appoint a single pharmacist leader to support improved prescribing.
- Action: Take at least one prescribing improvement action, such as requiring reassessment within 48 hours to check drug choice, dose, and duration.
- Tracking: Monitor prescribing and antibiotic resistance patterns.
- Reporting: Regularly report to staff prescribing and resistance patterns, and steps to improve.
- Education: Offer education about antibiotic resistance and improving prescribing practices.
- Work with other health care facilities to prevent infections, transmission, and resistance.
New Investment Needed
Expanding upon current patient safety efforts and goals, the FY 2015 President's Budget requests funding for CDC to increase the detection of antibiotic resistant infections and improve efforts to protect patients from infections, including those detailed in today's CDC reports. Additionally the President's Budget requests an increase for the National Healthcare Safety Network to fully implement tracking of antibiotic use and antibiotic resistance threats in U.S. hospitals.
- Page last reviewed: April 28, 2014
- Page last updated: April 28, 2014
- Content source:
- National Center for Emerging and Zoonotic Infectious Diseases
- Page maintained by: Office of the Associate Director for Communication, Digital Media Branch, Division of Public Affairs



 ShareCompartir
ShareCompartir