Do You Know About Thalassemia?
 Thalassemia is a serious condition that can lead to organ damage and even death. Find out more about related health problems treatment, CDC’s work, and what you can do to make a difference.
Thalassemia is a serious condition that can lead to organ damage and even death. Find out more about related health problems treatment, CDC’s work, and what you can do to make a difference.
Did you know that thalassemia is an inherited blood disorder that occurs because red blood cells from a person with thalassemia don't make enough of an important protein called hemoglobin? When there isn't enough hemoglobin, the body's red blood cells don't function properly and they last shorter periods of time, so there are fewer healthy red blood cells traveling in the bloodstream.
Red blood cells carry oxygen to all the cells of the body. Oxygen is a sort of food that cells use to function. When there are not enough healthy red blood cells, there is also not enough oxygen delivered to all the other cells of the body, which may cause a person to feel tired, weak or short of breath. This is a condition called anemia. People with thalassemia may have mild to severe anemia. Severe anemia can damage organs and lead to death.
In recognition of International Thalassemia Day, read below to learn more and find out what you can do to make a difference.
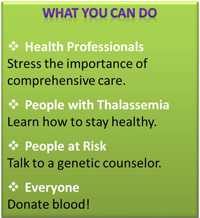 What You Can Do
What You Can Do
Health Professionals
Stress to your patients the importance of receiving comprehensive care. People with thalassemia, need to receive appropriate treatment in order to live a full and healthy life. Often, they will need several different kinds of healthcare professionals who work as a team to provide the best comprehensive treatment. Refer patients to a Thalassemia Treatment Center (TTC), which has in place a team of doctors, nurses, and other health professionals who have experience in treating people with thalassemia. Encourage patients to have a comprehensive care exam annually (bi-annually, in cases of less severe thalassemia) to monitor how treatment is going, learn what areas may need to be modified, etc.
People at Risk
Because the changes in the genes that cause thalassemia can be passed from parents to children, it is very hard to prevent. However, if you or your partner knows of family members with thalassemia, or if you both have family members from places in the world where thalassemia is common, you can speak to a genetic counselor to determine what the risk would be for your children to have thalassemia.
People with Thalassemia
A healthy lifestyle is important for everyone. For people living with thalassemia, it is especially important to know that a healthy lifestyle means "managing the disorder", as well as making healthy choices. Learn how now.
Everyone
People with thalassemia, as well as some other blood disorders need blood transfusions to stay healthy. You can make a difference by donating blood today. To find out where you can donate, click here.
Who is at Risk?
Because thalassemias are inherited, the condition sometimes runs in families. Some people find out about their thalassemia because they have relatives with a similar condition.
People who have family members from certain parts of the world have a higher risk for having thalassemia. Traits for thalassemia are more common in people from Mediterranean countries, like Greece and Turkey, and in people from Asia, Africa, and the Middle East. If you have anemia and you also have family members from these areas, your doctor might test your blood further to find out if you have thalassemia.
People with moderate and severe forms of thalassemia usually find out about their condition in childhood, since they have symptoms of severe anemia early in life. People with less severe forms of thalassemia may only find out because they are having symptoms of anemia, or maybe because a doctor finds mild anemia on a routine blood test or a test done for another reason.
 Treatments
Treatments
The type of treatment a person receives depends on how severe the thalassemia is. The more severe the thalassemia, the less hemoglobin the body has, and the more severe the anemia may be.
One way to treat anemia is to provide the body with more red blood cells to carry oxygen. This can be done through a blood transfusion, a safe, common procedure in which you receive blood through a small plastic tube inserted into one of your blood vessels. Some people with thalassemia – usually with thalassemia major –need regular blood transfusions because their body makes such low amounts of hemoglobin. People with thalassemia intermedia (not as severe as major, but not as mild as trait) may need blood transfusions sometimes, such as when they have an infection or an illness. People with thalassemia minor or trait usually do not need blood transfusions because they either do not have anemia or have only a mild anemia.
Many times people with thalassemia are prescribed a supplemental B vitamin, known as folic acid, to help treat anemia. Folic acid can help red blood cells develop. Treatment with folic acid is usually done in addition to other therapies.
CDC at Work – Monitoring the Nation's Blood Supply
People with inherited blood disorders like thalassemia often require frequent blood transfusions to remain healthy. In the United States, blood donations are screened for various viruses that can cause infections. Additionally, blood donors can be excluded from donating based on their responses to questionnaires to determine their risk of having a transfusion-transmissible infection (an infection that can be passed to another person through a blood transfusion). These mechanisms work together to keep the risk of obtaining a transfusion-transmitted infection extremely low.
Epidemiology and Surveillance
In 2004, CDC started the Thalassemia Data and Blood Specimen Collection System to quickly find infections that might be spread through blood transfusion. It focused on patients receiving care at seven CDC-funded Thalassemia Treatment Centers. Participants were tested each year for the presence of hepatitis, human immunodeficiency virus (HIV), and West Nile virus.
In 2012, the CDC expanded monitoring to include other heavily transfused populations (e.g., persons with sickle cell disease) with a project called Blood Safety Surveillance for People with Blood Disorders. This project helps to monitor those who receive repeated transfusions of red blood cells that may have a virus, and through the monitoring, increase the likelihood that a new or emerging threat to the safety of blood can be found quickly. In addition to hepatitis and HIV, the new project focuses on new and emerging threats to blood safety and other harmful effects of repeated blood transfusion (such as alloimmunization or iron overload).
Publications from Thalassemia Data on Blood Safety
The data from the Thalassemia Data and Blood Specimen Collection System has been analyzed and published in two articles. One was published in the journal AIDS Research and Human Retroviruses titled "Human T Cell Lymphotropic Virus Type 1 Infection Among U.S. Thalassemia Patient". The other was published in the journal Transfusion titled "Transfusion Complications in Thalassemia Patients: A Report from the Centers for Disease Control and Prevention (CDC)". The results of these two reports highlight the continued importance of monitoring and screening the nation's blood supply to decrease transfusion-related health risks.
More Information
- Page last reviewed: May 5, 2014
- Page last updated: May 5, 2014
- Content source:
- National Center on Birth Defects and Developmental Disabilities
- Page maintained by: Office of the Associate Director for Communication, Digital Media Branch, Division of Public Affairs



 ShareCompartir
ShareCompartir