Hepatitis E FAQs for Health Professionals
Index of Questions
Overview and Statistics
What is Hepatitis E?
Hepatitis E is a liver disease caused by the Hepatitis E virus (HEV). HEV infection usually results in a self-limited, acute illness. It is widespread in the developing world. Although rare in developed countries, locally acquired HEV infection can result in acute hepatitis with tendency to progress to chronic hepatitis mainly among solid organ transplant recipients.
How common is Hepatitis E in the United States?
Hepatitis E is believed to be uncommon in the United States. However, some studies have found a high prevalence of antibodies to HEV in the general population. When symptomatic hepatitis E does occur, it is usually the result of travel to a developing country where hepatitis E is endemic. Increasingly, sporadic Hepatitis E cases not associated with travel have been identified in developed countries. No clear exposure was identified for these domestically acquired (non-travel related) cases.
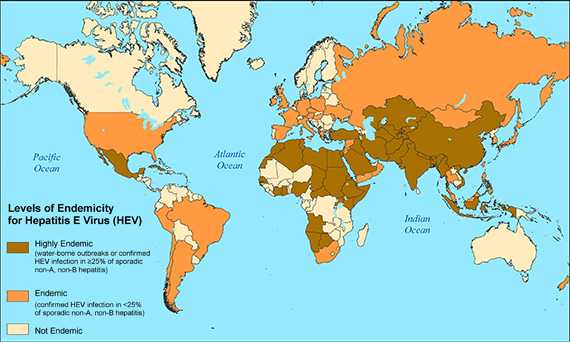
Where is Hepatitis E most common?
Hepatitis E is most common in developing countries with inadequate water supply and environmental sanitation. Large hepatitis E epidemics have been reported in Asia, the Middle East, Africa, and Central America. People living in refugee camps or overcrowded temporary housing after natural disasters can be particularly at-risk.
Are there different genotypes of Hepatitis E and where can they be found?
The unique characteristics of HEV is that it displays different clinical and epidemiologic profile depending on where the infection is acquired which is mainly due to the viral genotype. There are four genotypes of HEV, each displaying different epidemiological and clinical characteristics between developing and developed countries. Cases of Hepatitis E typically present in one of two ways, either as large outbreaks and sporadic cases in area where HEV is endemic (genotype 1 in Asia and Africa, genotype 2 in Mexico and west Africa and genotype 4 in Taiwan and China) or as isolated cases in developed countries (genotype 3).
| Characteristics | Genotype 1 | Genotype 2 | Genotype 3 | Genotype 4 |
|---|---|---|---|---|
| Geographic Location | Africa and Asia | Mexico, West Africa | Developed Countries | China, Taiwan, Japan |
| Transmission route | Water-borne Fecal- oral Person to Person | Water-borne Fecal-oral | Food-borne | Food-borne |
| Groups at high risk for infection | Young Adults | Young Adults | Older Adults (>40 years) and Males Immuno-compromised persons |
Young Adults |
| Zoonotic transmission | No | No | Yes | Yes |
| Chronic Infection | No | No | Yes | No |
| Occurrence of Outbreaks | Common | Smaller scale outbreaks | Uncommon | Uncommon |
Transmission and Exposure
How is the Hepatitis E virus spread?
Hepatitis E virus is usually spread by the fecal-oral route. The most common source of HEV infection is fecally contaminated drinking water. In developing countries, HEV genotypes 1 and 2 are spread by fecally contaminated drinking water.
In developed countries sporadic cases of HEV genotype 3 have occurred following consumption of uncooked/undercooked pork or deer meat. Consumption of shellfish was a risk factor in a recently described outbreak in a cruise ship. HEV genotype 4, detected in China, Taiwan, and Japan, has also been associated with foodborne transmission.
Can the Hepatitis E virus be spread by animals?
There is a possibility of zoonotic spread of the virus. HEV RNA (genotypes 3 and 4) had been extracted from pork, boar, and deer meat. Foodborne infection, could occur from consumption of uncooked/undercooked meat or organs from infected animals.
Symptoms
What are the signs and symptoms of Hepatitis E?
When they occur, the signs and symptoms of Hepatitis E are similar to those of other types of acute viral hepatitis and can include:
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Jaundice
- Dark urine
- Clay-colored stool
- Joint pain
The ratio of symptomatic to asymptomatic infection ranges from 1:2 to 1:13.
Who is most likely to have symptomatic HEV infection?
Symptomatic Hepatitis E in developing countries commonly occurs among older adolescents and young adults (aged 15–44 years). Pregnant women are more likely to experience severe illness including fulminant hepatitis and death.
In developed countries, sporadic cases due to HEV genotype 3 mainly affect older men (>40 years of age). Acute and chronic HEV infection occur in solid organ transplant recipients on immunosuppressant therapy.
How soon after exposure will symptoms appear?
When symptoms occur, they usually develop 15 to 60 days (mean: 40 days) after exposure.
How long does an HEV-infected person remain infectious?
The period of infectiousness has not been clearly determined, but virus excretion in stool has been demonstrated from one week prior to onset up to 30 days after the onset of jaundice. Chronically infected persons shed virus as long as infected.
How serious is Hepatitis E?
Most people with Hepatitis E recover completely. During HEV outbreaks, the overall case-fatality rate is about 1%. However, for pregnant women, Hepatitis E can be a serious illness with mortality reaching 10%–30% in their third trimester of pregnancy. Hepatitis E could also be serious among persons with preexisting chronic liver disease resulting in decompensated liver disease and death. Similarly high mortality occurs solid organ transplant recipients on immunosuppressive therapy.
Can Hepatitis E become chronic?
To date, there is no report of progression of acute hepatitis E to chronic Hepatitis E in developing countries where HEV genotypes 1 and 2 are the predominant causes of illness. However, more and more cases of Hepatitis E with progression to chronic hepatitis and chronic liver disease are being reported among HEV genotype 3 cases acquired in the developed countries. These chronic cases are exclusively among persons who are on immunosuppressive treatment for solid organ transplant.
Diagnosis and Treatment
How is Hepatitis E diagnosed?
Because cases of Hepatitis E are not clinically distinguishable from other types of acute viral hepatitis, diagnosis can be confirmed only by testing for the presence of antibody against HEV or HEV RNA.
No serologic tests to diagnose HEV infection have been approved by FDA for use in the United States. Several tests are available for research purposes and some commercial laboratories use commercially available assays from other countries.
HEV infection should be considered in any person with symptoms of viral hepatitis who has traveled to a hepatitis E endemic region, recently travelled from an endemic area, or from an outbreak afflicted region and who is negative for serologic markers of Hepatitis A, B, C, and other hepatotropic viruses. A detailed history regarding sources of drinking water, uncooked food, and contact with jaundiced persons should be obtained to aid in diagnosis. There are increasing numbers of domestically acquired cases of hepatitis E and diagnosis should be suspected when no etiology can be identified on thorough evaluation.
Where can I learn more about hepatitis E serology?
CDC offers an online training that covers the serology of hepatitis E and other types of viral hepatitis, available at https://www.cdc.gov/hepatitis/resources/professionals/training/serology/training.htm.
How is Hepatitis E treated?
Hepatitis E usually resolves on its own without treatment. There is no specific antiviral therapy for acute Hepatitis E. Physicians should offer supportive therapy. Patients are typically advised to rest, get adequate nutrition and fluids, avoid alcohol, and check with their physician before taking any medications that can damage the liver, especially acetaminophen. Hospitalization is sometimes required in severe cases and should be considered for pregnant women.
Few case reports and case series have indicated that modification of immunosuppressive medication and/or use of antiviral drugs may result in spontaneous viral clearance in immunocompromised patients with chronic hepatitis E.
Prevention
How is Hepatitis E prevented?
Prevention of Hepatitis E relies primarily on good sanitation and the availability of clean drinking water. Travelers to developing countries can reduce their risk for infection by not drinking unpurified water. Boiling and chlorination of water will inactivate HEV. Avoiding raw pork and venison can reduce the risk of HEV genotype 3 transmission.
Immune globulin is not effective in preventing Hepatitis E.
Is there a vaccine for Hepatitis E?
No FDA-approved vaccine for Hepatitis E is currently available in the United States; however, a recombinant vaccine was recently approved for use in China.
- Page last reviewed: July 10, 2017
- Page last updated: December 18, 2015
- Content source:


 ShareCompartir
ShareCompartir