Asian Americans and Pacific Islanders and Chronic Hepatitis B
Key Facts
- Asian Americans and Pacific Islanders (AAPIs) make up less than 5% of the total population in the United States, but account for more than 50% of nearly one million Americans living with chronic hepatitis B.
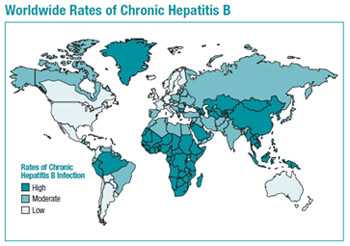
- The burden of chronic hepatitis B in the US is greater among people born in regions of the world with high or moderate prevalence of chronic hepatitis B, including much of Asia and the Pacific Islands.
- Nearly 70% of Asian Americans are foreign-born and estimates have found that approximately 58% of foreign-born people with chronic hepatitis B are from Asia
- Left untreated, approximately 15% to 25% of those with chronic hepatitis B infection develop serious liver disease, including cirrhosis, liver damage, and even liver cancer
- Asian Americans and Pacific Islanders are 8-13 times more likely to develop liver cancer than other groups, primarily due to hepatitis B infection
- The liver cancer death rate is 60% higher for Asian Americans and Pacific Islanders than Caucasians
Hepatitis B Testing Recommendation for Asian Americans and Pacific Islanders
CDC recommend testing the following groups for hepatitis B:
- All people born in regions of the world with high or moderate rates of hepatitis B. This includes all countries in Asia and the Pacific Islands
- All people born in the United States, who were not vaccinated at birth, and who have at least one parent born in a country with high hepatitis B rates. This includes all countries in East and Southeast Asia, except for Japan, and the Pacific Islands
- Household contacts and sexual partners of people with hepatitis B.
For additional information on other groups that should be tested for hepatitis B, see: Recommendations for Identification and Public Health Management of Persons with Chronic Hepatitis B Virus Infection [PDF - 28 pages]
Rationale for the Recommendation
- At least one-third of Asian Americans living in the United States are unaware of their chronic hepatitis B infection
- Prompt identification of chronic hepatitis B infection is essential to ensure infected people receive necessary care to prevent or delay onset of liver disease and services to prevent transmission to others
- Chronically infected patients have years of life to gain if medical evaluation and/or treatment is initiated early, before symptoms occur
- Multiple medications have been approved for treatment of adults with chronic hepatitis B
- Identifying people with chronic hepatitis B also allows for primary and secondary prevention. Close contacts can benefit from vaccination if never infected, or medical management if living chronic hepatitis B.
Guidelines and Recommendations
Chronic Hepatitis B Testing
- Recommendations for Identification and Public Health Management of Persons with Chronic Hepatitis B Virus Infection [PDF 28 pages]
- U.S. Preventative Services Task Force (USPSTF) – Screening for Hepatitis B Virus Infection
- American Association for the Study of Liver Diseases (AASLD) – Chronic Hepatitis B [PDF - 38 pages]
Hepatitis B Vaccination
- A Comprehensive Immunization Strategy to Eliminate Transmission of Hepatitis B Virus Infection in the United States
Part 1: Immunization of Infants, Children, and Adolescents [PDF - 39 pages]
Part 2: Immunization of Adults [PDF - 40 pages]
Healthcare Provider Resources
- Testing Asian Americans and Pacific Islanders for Hepatitis B [PDF - 2 pages]
- Geographic Distribution of Chronic Hepatitis B virus (HBV) Infection [PDF - 1 page]
- Hepatitis B Information for Health Professionals
- Testing Recommendations for Chronic Hepatitis B Virus Infection
- Recommendations for Routine Testing and Follow-up for Chronic Hepatitis B Virus Infection [PDF - 2 pages]
- Interpretation of Hepatitis B Serologic Test Results [PDF - 1 page]
Patient Resources
- Hepatitis B Patient Education Resources -- http://www.cdc.gov/hepatitis/HBV/PatientEduB.htm
- CDC’s Know Hepatitis B campaign, targeting AAPIs to get tested for hepatitis B -- http://www.cdc.gov/knowhepatitisB/
- Page last reviewed: August 30, 2016
- Page last updated: August 30, 2016
- Content source:


 ShareCompartir
ShareCompartir