Investigation Announcement: Multistate Outbreak of Salmonella Enteritidis Infections Linked to Restaurant Chain A
January 19, 2012 (FINAL Update)
On this Page
Introduction
CDC collaborated with public health officials in multiple states and the U.S. Food and Drug Administration (FDA) to investigate a multistate outbreak of Salmonella Enteritidis infections which was associated with eating food from a Mexican-style fast food restaurant chain, Restaurant Chain A. Investigative efforts were unable to identify a specific food associated with illness, but data indicate that contamination likely occurred before the product reached Restaurant Chain A locations. This outbreak now appears to be over.
Public health investigators used DNA "fingerprints" of Salmonella bacteria obtained through diagnostic testing with pulsed-field gel electrophoresis, or PFGE, to identify cases of illness that may be part of this outbreak. They used data from PulseNet, the national subtyping network made up of state and local public health laboratories and federal food regulatory laboratories that performs molecular surveillance of foodborne infections. The PFGE pattern in the outbreak has been seen before in PulseNet, and in the past typically caused 2-3 cases per month.
A widely distributed contaminated food product might cause illnesses in a specific region and across the United States. As of January 19, 2012, a total of 68 individuals infected with the outbreak strain of Salmonella Enteritidis have been reported from 10 states. The number of ill persons identified in each state with the outbreak strain was as follows: Texas (43), Oklahoma (16), Kansas (2), Iowa (1), Michigan (1), Missouri (1), Nebraska (1), New Mexico (1), Ohio (1), and Tennessee (1).
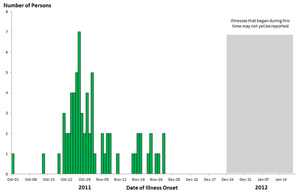
Among persons for whom information was available, illnesses began on or after October 13, 2011. Ill persons range in age from <1 to 79 years, and the median age was 25 years old. Fifty-four percent of patients were female. Thirty-one percent of patients were hospitalized. No deaths were reported.
The outbreak can be visually described with a chart showing the number of people who became ill each day. This chart is called an epi curve. Please see the Timeline for Reporting of Salmonella Cases for more details.
Investigation of the Outbreak
Collaborative investigative efforts of state, local, and federal public health agencies indicated that eating food from a Mexican-style fast food restaurant chain, Restaurant Chain A, was associated with some illnesses. Public health officials in multiple states and CDC conducted interviews with ill persons to ask questions about exposures during the days before becoming ill. Among 52 ill persons for whom information is available, 60% reported eating at Restaurant Chain A in the week before illness onset. Ill persons reported eating at 18 different locations of Restaurant Chain A in the week before becoming ill. A total of 3 locations were identified where more than one ill person reported eating in the week before becoming ill. This finding indicates that contamination likely occurred before the product reached Restaurant Chain A locations.
CDC and public health officials in multiple states conducted an epidemiologic study by comparing foods eaten by 48 ill and 103 well persons. Analysis of this study indicates that eating at Mexican-style fast food Restaurant Chain A was associated with illness. Ill persons (62%) were significantly more likely than well persons (17%) to report eating at Restaurant Chain A in the week before illness. No specific food item or ingredient was found to be associated with illness due to common ingredients being used together in many menu items. However, among ill persons eating at Restaurant Chain A, 90% reported eating lettuce, 94% reported eating ground beef, 77% reported eating cheese, and 35% reported eating tomatoes. The epidemic curve seen in the outbreak is consistent with those observed in past produce-related outbreaks—with a sharp increase and decline of ill persons that spanned one to two months. Ground beef was an unlikely source due to the handling and cooking processes used by Restaurant Chain A.
FDA used information on supply truck delivery routes and schedules to try to identify potential foods associated with reports of illness. FDA collected and analyzed paper and electronic shipping records of suspected foods and various other food products shipped by a food distribution center to Restaurant Chain A locations. After reviewing these records, FDA found locations where more than one ill person reported eating in the week before becoming ill were on two separate trucking routes. Comparison of records from suspected foods received by these locations revealed no commonalities across a variety of suppliers. Despite these additional efforts, no further information was available to assist in identifying a single food item.
Restaurant Chain A, as well as their food suppliers and distributors, were very cooperative in providing extensive information to public health officials as various leads were explored.
This particular outbreak appears to be over. However, Salmonella is still an important cause of human illness in the United States. More information about Salmonella, and steps people can take to reduce their risk of infection, can be found on the CDC Salmonella Web Page and the CDC Vital Signs Web Page.
Clinical Features/Signs and Symptoms
Most persons infected with Salmonella bacteria develop diarrhea, fever, and abdominal cramps 12 to 72 hours after infection. The illness usually lasts 4 to 7 days, and most persons recover without treatment. However, in some persons, the diarrhea may be so severe that the patient needs to be hospitalized. Salmonella infection may spread from the intestines to the bloodstream and then to other body sites and can cause death unless the person is treated promptly with antibiotics. Older adults, infants, and those with impaired immune systems are more likely to have a severe illness from Salmonella infection. More information about Salmonella, and steps people can take to reduce their risk of infection with Salmonella in general, can be found on the CDC Salmonella Web Page and the CDC Vital Signs Web Page.
Advice to Consumers, Retailers, and Others
- At this time, there is no specific advice to consumers.
- Consumers are not warned to avoid any specific foods or restaurants.
- If a food source is identified for this outbreak and if there is evidence of continued risk of infection, public health officials will advise the public and take the necessary steps to avoid risk of additional illnesses.
- To facilitate successful traceback efforts and outbreak investigations, retail establishments should maintain detailed records of food suppliers and distributors.
CDC's Role in Food Safety
CDC leads federal efforts to gather data on foodborne illnesses, investigate foodborne outbreaks and monitor the effectiveness of prevention and control efforts. CDC is not a food safety regulatory agency but works closely with the food safety regulatory agencies, in particular, with FDA and U.S. Department of Agriculture's Food Safety and Inspection Service. CDC also plays a key role in building state and local health department epidemiology, laboratory and environmental health capacity to support foodborne disease surveillance and outbreak response. Notably, CDC data can be used to help document the effectiveness of regulatory interventions.
Get email updates
To receive email updates about this page, enter your email address:
Contact Us:
- Centers for Disease Control and Prevention
1600 Clifton Rd
Atlanta, GA 30333 - 800-CDC-INFO
(800-232-4636)
TTY: (888) 232-6348 - Contact CDC–INFO