Healthcare-Associated Infections (HAIs)
Healthcare-associated infections (HAIs) are complications of healthcare and linked with high morbidity and mortality. Each year, about 1 in 25 U.S. hospital patients is diagnosed with at least one infection related to hospital care alone; additional infections occur in other healthcare settings. Many HAIs are caused by the most urgent and serious antibiotic-resistant (AR) bacteria and may lead to sepsis or death. CDC uses data for action to prevent infections, improve antibiotic use, and protect patients.
- 50 percent decrease in central line-associated bloodstream infections (CLABSI) between 2008 and 20143
- 36 percent decrease in healthcare-associated invasive MRSA, 2008–2014. In addition, National Healthcare Safety Network (NHSN) data reported a 13% decrease (2011 – 2014) for hospital-onset MRSA bacteremia bloodstream infections, confirming overall trends.
- 17 percent decrease in select surgical site infections (SSI)
- 8 percent decrease in hospital-onset Clostridium difficile (C. difficile) infections between 2011 and 2014
- 24 percent decrease in CAUTI in acute care hospital wards, 2009 – 2014, and 16 percent increase in CAUTI in hospital intensive care units.4
Progress in healthcare-associated infections
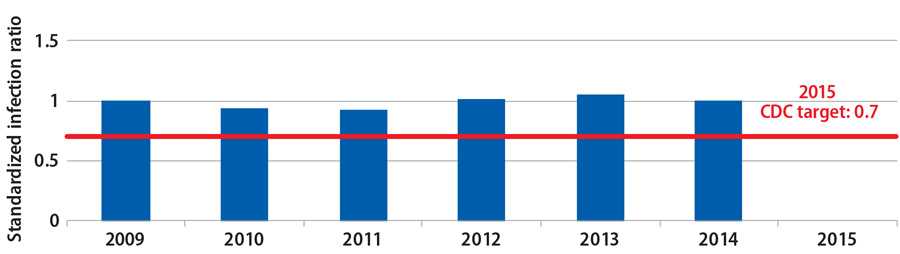
SIR for central line-associated bloodstream infections declined sharply

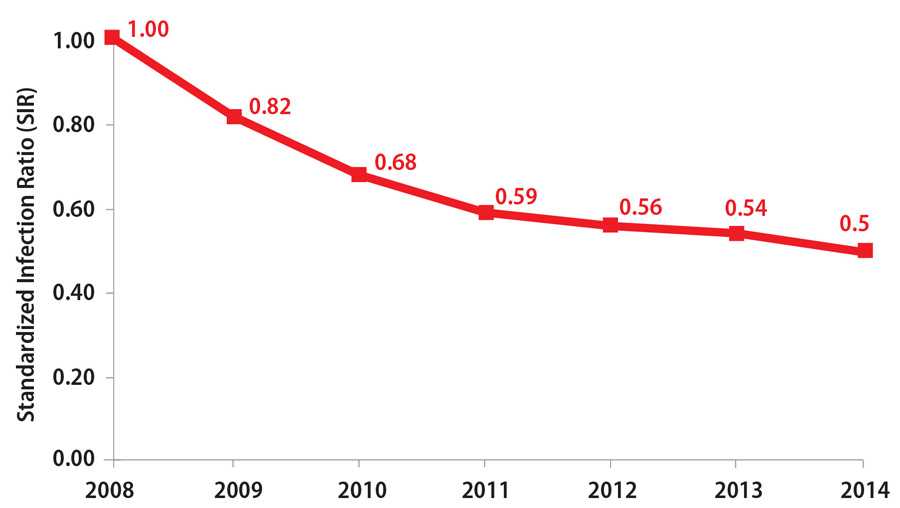
National and State Healthcare-associated Infections Progress Report, published January 2016, based on 2014 data;
www.cdc.gov/hai/surveillance/progress-report/index.html
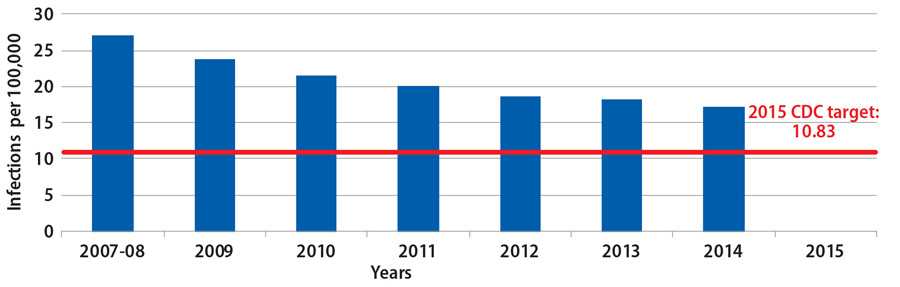
Trends in catheter-associated urinary tract infections (CAUTI) in hospitals 2009 – 20144
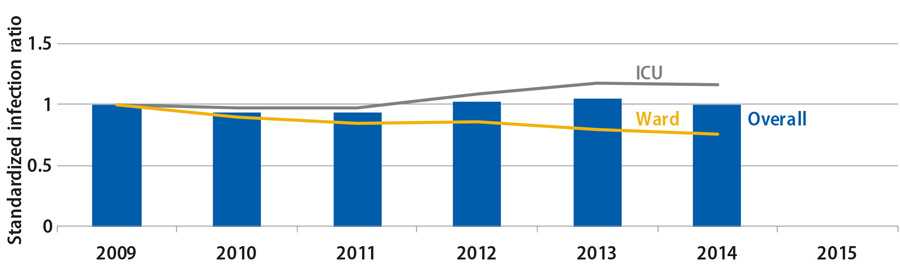
Source: CDC’s National Healthcare Safety Network (NHSN)
3 CLABSI data reflect progress in acute-care hospitals only.
4 CAUTI data reflect progress in acute-care hospitals only. Although 2009 – 2014 data show no change in overall CAUTI SIRs, specific hospital units showed major
changes in CAUTI SIRs: 24% decrease in hospital wards and 16% increase in hospital intensive care units (ICUs).
Trends in Healthcare-Associated Infections Winnable Battle Indicators
Trends in central line-associated blood stream infections (CLABSI) in hospitals, 2006 – 20143
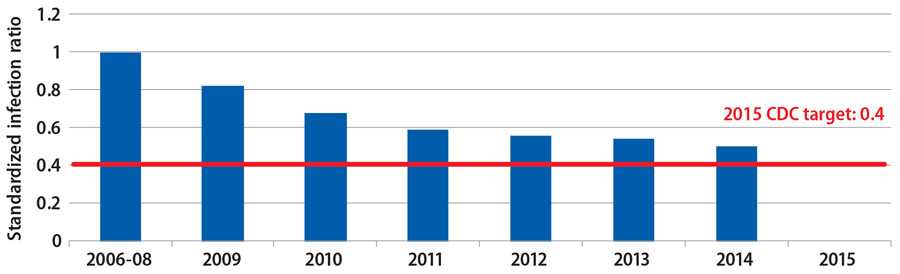
Source: CDC’s National Healthcare Safety Network (NHSN)
3 CLABSI data reflect progress in acute-care hospitals only.
Trends in surgical site infections (SSI) in hospitals, 2006 – 2014
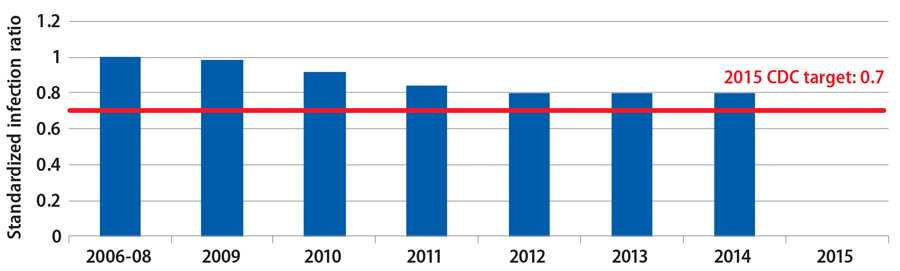
Source: CDC’s National Healthcare Safety Network (NHSN)
Trends in catheter-associated urinary tract infections (CAUTI) in hospitals, 2009 – 20144
Source: CDC’s National Healthcare Safety Network (NHSN)
4 CAUTI data reflect progress in acute-care hospitals only. Although 2009 – 2014 data show no change in overall CAUTI SIRs, specific hospital units showed major changes in CAUTI SIRs: 24% decrease in hospital wards and 16% increase in hospital intensive care units (ICUs).
Trends in healthcare-associated invasive methilicillin-resistant Staphylococcus aureus (MRSA) infections, 2007 – 20145
Source: Emerging Infections Program / Active Bacterial Core Surveillance
5 Starting in 2015, the MRSA data source will be Emerging Infections Program / Healthcare-Associated Infections Component (EIP / HAIC) and National
Healthcare Safety Network (NHSN).

Considerations in Choosing Healthcare-Associated Infections as Winnable Battle
- CDC had a long history of tracking HAIs as well as developing and promoting evidence-based recommendations for infection prevention and control, but many infections were not being prevented.
- In the early 2000s, evidence indicated that full adherence to CDC guidelines prevented 70% of CLABSIs in some hospitals; however, too many infections were still occurring.
- In 2009, the federal government added commitment to HAI prevention with the establishment of national prevention goals with the National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination using CDC’s National Healthcare Safety Network (NHSN) to track progress. In addition, for the first time, states received limited funding to support developing infrastructure that could promote and assist in HAI prevention efforts.
- This combination of CDC data, guidelines, national goals, and new state support provided a unique opportunity to make major gains in reducing — and in some cases, eliminating — HAIs.
Challenges / Obstacles
- We needed to develop a new normal in which HAIs are considered unacceptable and rare events in healthcare.
- We needed commitment from traditional and new public health and healthcare stakeholders at all levels — federal, state, local, health system, healthcare provider, and patient — as well as public and private sectors to make an impact.
- There was a need among many stakeholders to embrace more transparency and accountability.
State Spotlight: Tennessee Reduces HAIs Using Data for Action
Tennessee has made significant progress preventing HAIs by intensely focusing on using actionable NHSN data to drive improvement in healthcare. Tennessee started in 2008 as one of only two states in the country with a CLABSI SIR significantly higher than the national baseline, and by 2014, the state had reduced CLABSIs to 52% below the national baseline.
The Tennessee Department of Health (TDH) HAI & AR (Antibiotic Resistance) Program achieved this by turning to its data: collecting, verifying, and then acting on hospital data to compare facilities, identify where infections were occurring, and then focus targeted prevention in specific facilities in the state and locations within the facility.
Such aggressive action was not possible without TDH’s strong partnerships. HAI prevention was integrated into work with CMS-funded networks, state hospital associations, and other local partners to establish priorities, set goals, align strategies, and clearly define roles and responsibilities.
“We’ve embraced the TAP strategy in Tennessee for several reasons. We feel it has the greatest return on investment, by targeting facilities with the potential to prevent the greatest number of infections,” said Dr. Marion Kainer, TDH HAI Program Director.
TDH is a state leader in HAI / AR prevention. In fact, CDC worked with TDH to adapt this early strategy into CDC’s TAP strategy, now available nationwide with NHSN data tools. TDH is now working to expand its successful approach across the spectrum of healthcare and HAI / AR threats in the state.
CDC Contributions in Healthcare-Associated Infections Winnable Battle
Since 2008, the combination of CDC data systems, evidence-based recommendations, public health-healthcare programs, and partnerships have contributed to significant reductions of HAIs across healthcare settings. CDC focuses its prevention efforts on major device- and procedure-related HAIs, as well as controlling the spread of infections.
Using Data for Action: Transparency and Accountability
CDC promotes the use of HAI / AR data for action to identify gaps in infection prevention, set goals for prevention, and prioritize interventions for public health impact. Partners use CDC’s data systems and data-based tools and resources to drive quality improvement in healthcare.
- CDC’s National Healthcare Safety Network (NHSN) is the nation’s most widely used system to track HAIs. Facilities use NHSN to not only fulfill federal and state reporting requirements, but also act on their NHSN data to monitor and prevent infections within their facilities. In collaboration with CMS and state partners, CDC increased the number of healthcare facilities reporting to NHSN from ~1,800 to 19,000.
- Every year, CDC releases publicly available data and information on state, regional, and national HAI / AR trends and illustrates progress toward the ultimate goal of eliminating HAIs. These resources include the annual National and State HAI Progress Report, CDC’s AR Threat Report (2013), and CDC’s AR Patient Safety Atlas (2016).
- CDC started to look at its data and public health impact differently. Not only did CDC continue to estimate disease burden, but CDC also began to assess numbers of infections prevented, lives saved, and medical costs averted through HAI prevention (CDC Vital Signs: Reducing Bloodstream Infections, 2011).
- To increase the use of data for prevention, CDC developed the Targeted Assessment for Prevention (TAP) strategy in 2015 to use NHSN data to identify healthcare facilities and within-facility units with disproportionately high HAI burden and target infection prevention efforts to those locations. TAP reports — currently available for CLABSI, CAUTI, and C. difficile infections — are used by CMS-funded networks (e.g., Quality Improvement Networks), health departments, and health systems and facilities across the country to work towards achieving specific HAI reduction goals.
- CDC identifies gaps where more interventions are needed or where CDC needs to find better ways to collect data. For example, using CDC’s NHSN and Emerging Infections Program data, CDC identified the new, emerging AR threats of C. difficile and CRE. CDC issued call-to-action Vital Signs reports alerting the nation to these rising threats and identifying concrete actions the public health-healthcare community could take to combat them (CDC Vital Signs: Stopping C. difficile Infections, 2012, and CDC Vital Signs: Stop Infections from Lethal CRE Germs Now, 2013).

Developing Innovative Approaches to Prevention
Wherever CDC works to detect and respond to HAI / AR outbreaks, prevent infections, stop spread of bacteria between patients, and improve antibiotic use, CDC looks to continually improve and develop innovative approaches to maximize public health impact.
- With academic applied research partners in CDC’s Prevention Epicenter Program, CDC identifies and tests new strategies for infection prevention and control, as well as clinical practice. For example, CDC worked with Chicago-area long-term acute care hospitals to evaluate a novel intervention bundle designed to stop the spread of CRE, finding it reduced CRE bloodstream infections by 56%. Likewise, the CDC-designed nationwide REDUCE MRSA Trial demonstrated that one strategy reduced bloodstream infections by up to 44% and significantly reduced the presence of MRSA and other pathogens in ICUs. Now, these infection prevention strategies are adopted as best practices in healthcare settings across the nation.
- CDC communicates and promotes infection prevention measures we know work. For example, the public health community has long recognized that antibiotic use puts patients at risk for C. difficile infection. With historically high C. difficile rates, CDC combined science, policy, and communications to release the Core Elements of Hospital Antibiotic Stewardship Programs to show how hospital CEOs and medical officers can improve antibiotic use and protect patients in their facilities (CDC Vital Signs: Antibiotic Rx in Hospitals: Proceed with Caution, 2014). CDC has since published core elements of antibiotic stewardship in nursing homes (2015) and outpatient settings (2016, pending).
- To identify gaps and strategies to meet Winnable Battle goals, CDC expanded data analytical techniques to predict HAI / AR trends, identify new interventions, and inform program direction. For example, CDC used mathematical modeling to predict increases in HAI / AR infections and C. difficile over the next five years without immediate, nationwide improvements in infection control and antibiotic prescribing (CDC Vital Signs: Stop Spread of AR, 2015). This led CDC to partner with academic researchers to test interventions within public health-healthcare prevention networks. These partnerships put these findings into practice which, if successful, serve as models for HAI / AR prevention in other areas of the country. This work also provided evidence to support expanding State HAI / AR Prevention Programs to better prevent infections, stop spread, and improve antibiotic use.
- In response to the complexities of combating HAI / AR across healthcare settings and in the community, CDC is integrating its detection, response, and prevention strategies to better protect patients. CDC urges healthcare personnel to always follow infection control recommendations and stewardship to better protect patients from HAIs caused by AR (CDC Vital Signs: Protect Patients from AR, 2016). Many of the most urgent and serious AR bacteria threaten patients while they are being treated in healthcare facilities for other conditions, and may lead to sepsis or death (CDC Vital Signs: Think Sepsis. Time Matters, 2016).
Expanding Collaborations to Implement What We Know Works
CDC works with diverse public health and healthcare partners to align prevention goals, promote the use of CDC guidelines and data for action, and aggressively work to prevent HAIs and AR infections across the spectrum of care.
- CDC works with other federal agencies to align national prevention goals and integrate proven prevention strategies and measures into national policies to change infection control practice.
- CDC and CMS have collaborated closely to include infection prevention and control and antibiotic stewardship programs in revised Conditions of Participation in Medicare and Medicaid programs for acute care hospitals and long-term care facilities. CDC’s NHSN data and prevention tools are also used by CMS-funded Quality Improvement Networks.
- CDC leads the 2016–2017 HHS Agency Priority Goal (APG) to expand stewardship programs nationwide, and worked closely with the CMS-led APGs to reduce CLABSIs (2012–2013) and CAUTIs (2012– 2015) nationwide.
- CDC also works with FDA to protect patients and stop outbreaks from spreading in healthcare facilities. Often, these outbreaks result from either failures in infection control practices or contaminated equipment or medications.
- CDC works with state and local health departments to support local HAI / AR expertise and lab capacity to improve identification and response to emerging threats, like Candida auris and mcr-1, leading to synchronized action across healthcare and communities to quickly protect patients and control spread.
- These partnerships expand HAI / AR prevention and antibiotic stewardship programs to implement proven strategies to prevent infections and transmission across healthcare settings.
- CDC is also implementing more prevention networks — where public health and healthcare work together — in more states to better prevent infections, stop spread, and improve antibiotic use.
- CDC works with health systems, academic and professional organizations, and healthcare consumers to expand strategies for clinical practice and promote tools to prevent infections and stop spread of bacteria across facilities. Each year, CDC works with over 100 partners on the Get Smart About Antibiotics Campaign to raise awareness of the threat of AR and the importance of appropriate antibiotic prescribing and use.
In fiscal year 2016, Congress appropriated $160 million for CDC to fight AR, a testament to the urgent AR threat and highest levels of support for the ambitious public health actions outlined in the National Action Plan for Combating Antibiotic-Resistant Bacteria (2015). This is a substantial opportunity for state and local public health, academic, healthcare, and veterinary partners to accelerate our efforts to establish the new normal in which HAIs are considered unacceptable and rare events in healthcare.
- Page last reviewed: November 28, 2016
- Page last updated: November 28, 2016
- Content source:


 ShareCompartir
ShareCompartir