We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Aortic ultrasound
From WikEM
Contents
Background
- Aortic ultrasound should be utilized to assess for aneurysm or dissection
- Aneurysm is defined as 3cm (150% the upper limit of normal) at the level of the renal arteries (L1-2 vertebral body level)
- Risk of AAA rupture significantly increases at 5cm but should be ruled out in the proper clinical setting when >3cm
- AAA’s are most commonly infrarenal
- EM providers have an accuracy of 100% in assessing for AAA[1]
- An intimal flap is 67–80% sensitive and 99–100% specific for dissection[2]
Indications
- Classic triad for AAA is pain, hypotension, and pulsatile mass
Technique
5-Point Assessment
- Select probe
- Curvilinear/large convex probe (phased array probe may substitute)
- Location
- Start at the superior aspect of the abdomen below the xyphoid process
- Visualize aorta on the patient’s left, IVC on the right, and vertebral shadow posteriorly
- Transverse views
- Proximal aorta
- Mid-aorta
- Distal aorta
- Aortic bifurcation
- Longitudinal view
- Distal aorta (to assess for saccular aneurysms)
Findings
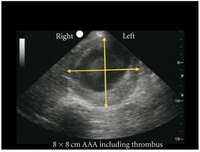
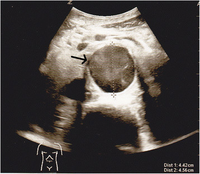
- AAA identified when diameter measured from outer wall to outer wall (including mural thrombus if present) is >3cm
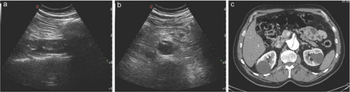
- Abdominal aortic dissection can be identified as an intimal flap
Images
Normal
Abnormal
Abdominal Aortic Aneurysm
Aortic Dissection
Pearls and Pitfalls
- Measurements should be done in a transverse view of the aorta for best wall to wall measurement
- Avoid oblique measurements which can be falsely large
- IVC can be differentiated by aorta as it is on the patient’s right, thin-walled, nonpulsatile, and compressible (depending on habitus)
- Constant gentle pressure and jiggling the probe can help to move bowel gas to visualize the aorta
- In the setting of ruptured AAA, blood may not show up in a fast exam if the bleeding is retroperitoneal
- AAA vs Dissection
- Dissections will continue while AAA typically are located in single area
- Dissections can be a normal diameter
- Mural thrombus can cause falsely small measurements
- Utrasound generally cannot differentiate ruptured from an intact AAA. The distinction is made based on clinical context.
Documentation
Normal Exam
A bedside ultrasound was conducted to assess for AAA with clinical indications of hypotension and lower back pain. The aorta was assessed at 4 locations in the transverse plane – proximal, mid, distal, and aortic bifurcation. Additionally, the distal aorta was viewed in the sagittal plane. No sonographic evidence of AAA at these sites.
Abnormal Exam
A bedside ultrasound was conducted to assess for AAA with clinical indications of hypotension and lower back pain. The aorta was assessed at 4 locations in the transverse plane – proximal, mid, distal, and aortic bifurcation. Additionally, the distal aorta was viewed in the sagittal plane. A 5.5cm AAA was discovered in the distal aorta.
Clips
External Links
See Also
References
- ↑ Kuhn M, Bonnin RL, Davey MJ, Rowland JL, et al. Emergency department ultrasound scanning for abdominal aortic aneurysm: accessible, accurate, and advantageous. Ann Emerg Med. 2000; 36(3):219-223.
- ↑ Fojtik JP, Costantino TG, Dean AJ. The diagnosis of aortic dissection by emergency medicine ultrasound. J Emerg Med. 2007; 32(2):191-196.