We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Diabetic ketoacidosis
From WikEM
(Redirected from Diabetic ketoacidosis (DKA))
Contents
Background
Epidemiology
- Mortality rate approximately 2-5%[1]
Pathophysiology
- Defining features include hyperglycemia (glucose > 250mg/dl), acidosis (pH < 7.3), and ketonemia/ketonuria
Hyperglycemia
- Leads to osmotic diuresis and depletion of electrolytes including sodium, magnesium, calcium and phosphorous.
- Further dehydration impairs glomerular filtration rate (GFR) and contributes to acute renal failure
Acidosis
- Due to lipolysis / accumulation of of ketoacids (represented by increased anion gap)
- Compensatory respiratory alkalosis (i.e. tachypnea and hyperpnea - Kussmaul breathing)
- Breakdown of adipose creates first acetoacetate leading to conversion to beta-hydroxybutyrate
Dehydration
- Causes activation of RAAS in addition to the osmotic diuresis
- Cation loss (in exchange for chloride) worsens metabolic acidosis
Clinical Features
History
- May be the initial presenting of an unrecognized T1DM patient
- Presenting signs/symptoms include altered mental status, tachypnea, abdominal pain, hypotension, decreased urine output.
- Perform a thorough neurologic exam (cerebral edema increases mortality significantly, especially in children)
- Assess for possible inciting cause (especially for ongoing infection; see Differential Diagnosis section)
Physical
- Ill appearance.
- Acetone breath.
- Drowsiness with decreased reflexes
- Tachypnea (Kussmaul's breathing)
- Signs of dehydration with dry mouth and dry mucosa.
- Perform a thorough neurologic exam as cerebral edema increases mortality significantly, especially in children
- There may be signs from underlying cause (eg pneumonia)
Differential Diagnosis
Causes of DKA
- Insulin or oral hypoglycemic medication non-compliance
- Infection
- Cardiac Ischemia
- Intra-abdominal infections
- Steroid use
- ETOH Abuse
- Drug abuse
- Pregnancy
- Hyperthyroidism
- GI Hemorrhage
- CVA
- PE
- Pancreatitis
- Renal Failure
- GI Bleed
- Alcoholic Ketoacidosis
Hyperglycemia
- Diabetic foot infection
- Diabetic ketoacidosis (DKA)
- Diabetic ketoacidosis (peds)
- Hemochromatosis
- Hyperosmolar hyperglycemic state (HONC)
- Iron toxicity
- New onset diabetes mellitus
- Nonketotic hyperglycemia
- Sepsis
Evaluation
- Diagnosis is made based on the presence of acidosis and ketonemia in the setting of diabetes.
- Strongly consider capnography for respiratory distress[2]
Workup
- CBC
- Blood glucose
- BMP
- Mag
- Phos
- Urinalysis
- VBG/ABG
- Beta-hydroxybutyrate
Blood Glucose
- Capillary blood sugar >250mg/dL
- Blood sugar may not be very elevated if there is impaired gluconeogenesis (eg liver failure, severe alcoholism) or patient is taking a SGLT-2 Inhibitor [3]
Blood Gas
- No need to perform Arterial blood gas. Venous blood gas is sufficient
- Difference in pH from VBG vs ABG will be ±0.02pH units[4][5] [6][7]
Elevated Anion Gap
- Bicarb may be normal due to compensatory and contraction alcoholosis so the elevated anion gap or ketonuria may be the only clues to the DKA
- VBG (equivalent to ABG for assessment of acid-base status)[8]
Serum ketones
- Beta hydroxybutyrate will be elevated
Urinary analysis (ketonuria)
- Note that urine dipstick may give a false negative for ketones since it does not detect beta-hydroxybutyrate
- As acetoacetate is converted to beta-hydroxybutyrate the urinary ketones may turn negative[9]
- Urinalysis will be positive very early in DKA
ECG
- Assessing for any cardiac dysfunction
Infectious evaluation
- This should be done as appropriate if the suspected underlying cause for DKA is an infection. (eg chest X-ray , blood cultures)
End Tidal CO2
- ETCO2 can be used for bedside assessment of DKA[10]
- An ETCO2 of ≥35 is 100% sensitive to rule out DKA
- An ETCO2 of ≤21 is 100% specific to diagnosis DKA
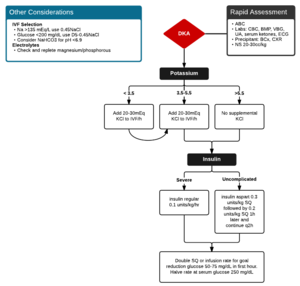
Management
Volume Repletion
- Administer 20-30cc/kg normal saline bolus during the first hour
- Most important step in treatment since osmotic diuresis is the major driving force[6]
- Most adult patients are 3-6L depleted
- Consider LRs to avoid worsening acidosis with contributory hyperchloremic metabolic acidosis[11]
- When blood sugar(BS) < 250 switch to Dextrose 5% 50-200ml/hr (+/- KCl)
Insulin Overview
- Check Potassium prior to insulin treatment![12]
- If potassium <3.5mEq/L, do not administer insulin until potassium supplementation is underway (to avoid worsening of hypokalemia)
- If potassium >3.5mEq/L and <5.5 mEq/L, start potassium repletion along with your insulin[13]
- A bolus dose is unnecessary and may contribute to increased hypoglycemic episodes[14]
- Expect BS to fall by 50-100mg/dL per hr if you administer 0.1units/kg/hr of insulin
- Refractory hyperglycemia may be due to an associated infectious process contributing to the DKA
IV Insulin Regimen
- Initial infusion 0.1units/kg/hr of insulin
- When BS <250mg/dL, halve the rate of infusion to 0.05units/kg/hr IV OR give subQ 0.1 U/kg q2hr and switch IV fluids to Dextrose 5% at 150cc/hr
- Maintain BS between 150 and 200mg/dL until resolution of acidosis
- May require IV fluids to be switched to Dextrose 10% when BS <150mg/dL
- Continue IV infusion for 2 hrs after subcutaneous insulin is begun
- SubQ route (appropriate only for mild DKA)
- Do not stop insulin infusion until AG normalized AND bicarb normalized, despite resolution of blood sugar. Aim of insulin regime is to correct the acidosis, not merely the hyperglycemia.
SubQ(SC) Insulin Regimen
A subcuntenous regemin must use short acting insulin and follow either a 1hr or 2hr dosing protocol. Regular insulin is not effective[15]
1hr Protocol
- Initial dose SC Aspart: 0.3 units/kg body wt, followed by
- SC aspart insulin at 0.1 units/kg every hour
- When blood glucose <250mg/dl (13.8 mmol/l), change IV fluids to D5<sub 0.45%NS and reduce SC aspart insulin to 0.05 units/kg/hr
- Keep glucose at 150mg/dl (11 mmol/l) until resolution of DKA.
2hr Protocol
- Initial dose SC Aspart: 0.3 units/kg body wt, followed by
- SC aspart insulin at 0.2 units/kg 1 hr later followed by Q2hr dosing
- When blood glucose <250mg/dl (13.8 mmol/l), change IV fluids to D5 0.45% saline and reduce SC aspart insulin to 0.1 units/kg/ 2hr
- Keep glucose at 150mg/dl (11 mmol/l) until resolution of DKA.
Electrolyte Repletion
- Potassium repletion is most important. Patients in DKA are almost always K+ depleted despite initially fairly normal K+. This is due to extracellular shift of K+ due to acidosis as well as insulin infusion, which increases uptake of K+ intracellularly.
- Sodium
- Hyponatremia may be due to translational hyponatraemia
- Na+ decreases by 1.6mEq/L for every 100mg/dL increase in glucose (ie pseudohyponatremia)
- Correction of glucose will result in normalization of Na+
- If truly hyponatraemic, start NS 250-500ml/hr
- If Hypernatremic then consider starting half-strength NS 250-500ml/hr after initial fluid bolus
- Hypophosphatemia: If < 1.0 mEq/L, start repletion.
- IV K2PO4 at 1mL/hour (contains 4.4meqK+ & 93mg phos)
- Severe hypophosphatemia can cause cardiac and respiratory dysfunction
- Hypomagnesemia – All patients who are hypokalemic are hypomagnesemic. Replete together as long as kidney function intact and if Mg<2.0mg/DL or symptoms suggest hypomagnesemia
- 2g MgSO4 IV over 1h
Bicarbonate[16]
- No evidence supports the use of sodium bicarb in DKA, with a pH >6.9
- However, no studies have been performed for patients with pH <6.9 and the most recent ADA guidelines recommend it for patients with pH <7.1
- Pitfalls of sodium bicarbonate therapy in DKA (outside of last ditch efforts in severe acidemia)[17]
- Paradoxical CSF acidosis
- Hypokalemia from H+ and K+ shifts
- Large sodium bolus
- Cerebral edema
- Shifts oxygen-hemoglobin dissociation curve to left, decreasing O2 delivery to tissues
Subsequent Management
Labs/Monitoring
- Glucose check Q1hr
- Chem 10 Q4hr (initially Q2hr)
- Check pH prn based on clinical status (eval respiratory compensation)
- Check appropriateness of insulin dose Q1hr (see below)
- Corrected Electrolytes
Sliding Scale
- Insulin Sliding Scale to be started once patient's DKA has resolved and eating a full diet.
Intubation
- Avoid intubation unless patient cannot generate respiratory alkalosis compensation due to extreme fatigue[18]
- Risks associated with intubation in DKA:
- During sedation/paralysis, a rise in PaCO2 can decrease pH considerably
- Severe gastroparesis in DKA creates a significant risk for aspiration
- Strong DKA patients generally can achieve greater hyperventilation than mechanical ventilated patients
- See Intubation for more information
Disposition
- Admit
Complications
See Also
- Diabetes mellitus (main)
- Evidence Review Sodium Bicarbonate in DKA
- Diabetic ketoacidosis (peds)
- Ketonemia
External Links
- British Society for Paediatric Endocrinology and Diabetes - Paediatric Diabetic Ketoacidosis
- DDxOf: Management of DIabetic Ketoacidosis
References
- ↑ Lebovitz HE: Diabetic ketoacidosis. Lancet 1995; 345: 767-772.
- ↑ Nagler J et al. Capnography: A valuable tool for airway management. Emerg Med Clin North Am, 26(4):881, Nov 2008.
- ↑ Peters AL et al. Euglycemic Diabetic Ketoacidosis: A Potential Complication of Treatment With Sodium-Glucose Cotransporter 2 Inhibition. Diabetes Care 2015 Sep; 38(9): 1687-1693.
- ↑ Kelly AM et al. Review Article – Can Venous Blood Gas Analysis Replace Arterial in Emergency Medical Care. Emery Med Australas 2010; 22: 493 – 498.
- ↑ Ma OJ et al. Arterial Blood Gas Results Rarely Influence Emergency Physician Management of Patients with Suspected Diabetic Ketoacidosis. Acad Emerg Med Aug 2003; 10(8): 836 – 41.
- ↑ 6.0 6.1 Savage MW, Datary KK, Culvert A, Ryman G, Rees JA, Courtney CH, Hilton L, Dyer PH, Hamersley MS; Joint British Diabetes Societies. Joint British Diabetes Societies guideline for the management of diabetic ketoacidosis. Diabet Med. 2011 May;28(5):508-15.
- ↑ Gokel Y, et al. Comparison of Blood Gas and Acid-Base Measurements in Arterial and Venous Blood Samples in Patients with Uremic Acidosis and Diabetic Ketoacidosis in the Emergency Room. American Journal of Nephrology 2000; 20:319-323.
- ↑ Ma OJ, Rush MD, Godfrey MM, Gaddis G. Arterial blood gas results rarely influence emergency physician management of patients
- ↑ Stojanovic, V. Sherri Ihle. Role of beta-hydroxybutyric acid in diabetic ketoacidosis: A review. Can Vet J. 2011 Apr; 52(4): 426–430.
- ↑ Chebl BR, Madden B, Belsky J, et al. Diagnostic value of end tidal capnography in patients with hyperglycemia in the emergency department. BCM Emerg Med. 2016; 16 (1).
- ↑ Van Zyl et al. Fluid Management in diabetic-acidosis--Ringer's lactate versus normal saline: a randomized controlled trial. http://qjmed.oxfordjournals.org/content/qjmed/105/4/337.full.pdf
- ↑ Aurora S, Cheng D, Wyler B, Menchine M. Prevalence of hypokalemia in ED patients with diabetic ketoacidosis. Am J Emerg Med 2012; 30: 481-4.
- ↑ *http://emupdates.com/2010/07/15/correction-of-critical-hypokalemia/
- ↑ Goyal N, Miller J, Sankey S, Mossallam U. Utility of Initial Bolus insulin in the treatment of diabetic ketoacidosis. Journal of Emergency Medicine, Vol 20:10, p30.
- ↑ Umpierrez G. et al. Treatment of diabetic ketoacidosis with subcutaneous insulin aspart. Diabetes Care. 2004 Aug;27(8):1873-8 [PDF http://care.diabetesjournals.org/content/27/8/1873.full.pdf]
- ↑ EBQ:Sodium Bicarbonate use in DKA
- ↑ Nickson C. Sodium Bicarbonate and Diabetic Ketoacidosis. Jan 28, 2014. http://lifeinthefastlane.com/ccc/sodium-bicarbonate-and-diabetic-ketoacidosis/.
- ↑ Four DKA Pearls. May 7, 2014. http://www.pulmcrit.org/2014/05/four-dka-pearls.html