We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Hyponatremia
From WikEM
Contents
Background
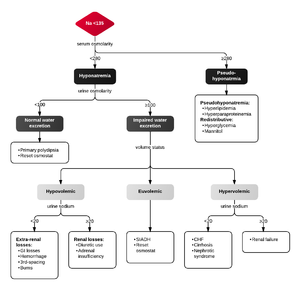
- Defined as sodium concentration <135meq/L[1]
- Patients often not symptomatic until <120meq/L although this level varies by patients and may be higher if the change occurred abruptly[2]
- Generally accepted recommendations are to avoid correction of more than 12 mmol/L/day (0.5mmol/L/hr) to avoid central pontine myelinolysis. Faster correction (1-2mmol/L/hr) is acceptable with 3% hypertonic saline if the patient is seizing.[3]
- Often described in terms of tonicity and volume status of the patient with the main types by tonicity being: [4]
- Hypertonic Hyponatremia
- Isotonic (pseudo) hyponatremia
- Hypotonic Hyponatremia
Clinical Features
- Nausea and Vomiting
- Anorexia
- Muscle cramps
- altered mental status
- Seizure (esp if Na < 113)
- Coma
- Rapid correction can cause CHF & CPM (altered mental status, dysphagia, dysarthria, paresis)
Hyponatremia Types by Tonicity
Hypertonic Hyponatremia
- Defined as osmolarity > 295mmol/L with the following causes:
- Hyperglycemia
- Traditional teaching: [Na+] decreases by 1.6-1.8mEq/L for each 100mg/dL increase in glucose over 100mg/dL
- 2.4mEq/L may be a more accurate correction factor (Hillier 1999)
- Mannitol excess
Isotonic (pseudo) hyponatremia
- Defined as osmolarity > 275-295mmol/L. Often referred to as pseudo hyponatremia because the elevated lipids or proteins interfere with the laboratory sodium reading. The following are common causes:
- Hyperlipidemia
- Hyperproteinemia
Hypotonic Hyponatremia
- Defined as an osmolarity < 275 mmol/L and categorized as hypovolemic, hypervolemic or euvolemic
Hypotonic Types by Volume Status
Hypovolemic
Renal Causes
- Thiazide diuretic use
- Na-wasting nephroathy (RTA, CRF)
- Osmotic diuresis (glucose, urea)
- Aldosterone deficiency
Extra-renal Causes
- GI loss
- 3rd space loss
- Burns
- Pancreatitis
- Peritonitis
Hypervolemic
- Urinary Na >20
- Urinary Na <20
Euvolemic
- SIADH
- urine sodium is greater than 20-40 mEq/L
- Pain, stress, nausea
- Psychogenic polydipsia
- Hypothyroidism
- Drugs[5]
- H20 intoxication
- Glucocorticoid deficiency
Pseudohyponatremia
- Hyperglycemia
- Na+ drops 1.6 mEq/L for every 100mg/dL increase in glucose over 100
- Displaced sodium in lab specimen
- Hyperlipidemia
- Hyperproteinemia
Evaluation
- Must determine volume status and calculated osm
- In true hyponatremia the osm is reduced
Work-Up
Prior to giving treatment
- Urine
- Urinalysis
- Urine electrolytes
- Urine urea
- urine uric acid
- urine osmolality
- urine creatinine
- Serum
- Chemistry
- Serum osmolality
- Uric acid
- TSH
- Cortisol
Treatment by Patient Status
Symptomatic
- Adults: 3% NS 100cc bolus over 10min; repeat after 10min x1 if no improvement[6]
- Each 100 ml will raise sodium by ~2 mmol/l
- In general, 200-400 mL of 3% NaCl is reasonable dose in most adult patients with severe symptomatic hyponatremia, which may be given IV over 1-2 hr until resolution of seizures.
- Pediatrics: 2 cc/kg of 3% over 10-60 minutes can be infused with a repeat of up to 3 times.[7]
- Fluid restrict
Asymptomatic
Step 1
Calculate total body water[8]
- TBW(kg) = Wt(kg) x 0.6 = [Wt(lb) x 0.45] x 0.6 = Wt(lb) x 0.27
Step 2
Calculate mEq deficit
- (Desired Na - Measured Na) ~ must be ≤ 10
Step 3
Calculate NS rate to be given over 24hr
- NS rate (cc/hr) = TBW x mEq deficit x 0.27
- If using 3% sodium chloride (to avoid volume overload) divide above rate by 3.33
Treatment by Type of Hyponatremia
Hypertonic hyponatremia
- Correct underlying disorder which is often hyperglycemia[9]
- Often volume depleted due to osmotic diuresis and normal saline provides adequate volume repletion
Isotonic (pseudo) hyponatremia
- No treatment needed [9]
Hypotonic hyponatremia
- Hypovolemic
- Give NS but be cautious of raising the serum sodium more than 12 mmol/L/day (0.5mmol/L/hr) and causing central pontine demylinosis[3]
- Euvolemic[9]
- Water restrict
- Treat underlying cause
- Hypervolemic
- Water restriction
- Diuresis
- Treat underlying cause
Na Therapy
Max correction 10mEq/L in first 24hr and 18mEq/L in first 48hr (lowers risk of central pontine demylinosis) [10]
| Fluid type | Sodium Concentration |
| 1/2 Normal Saline | 77 mEq/L |
| Normal Saline | 154 mEq/L |
| Lactated Ringers | 130 mEq/L |
| 3% Saline | 513 mEq/L |
Disposition
- Admit if symptomatic or if Na <125mEq/L
See Also
External Links
References
- ↑ Upadhyay A, Jaber BL, Madias NE. Epidemiology of hyponatremia. Seminars in Nephrology 2009 29 227–238
- ↑ Spasovski G. et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Nephrol Dial Transplant. 2014
- ↑ 3.0 3.1 Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000 May 25;342(21):1581-9.
- ↑ Understanding Lab Testing for Hyponatremia. Clin J Am Soc Nephrol 2008;3:1175
- ↑ Review of Drug-Induced Hyponatremia. Am J Kidney Dis 2008;52:144
- ↑ Spasovski et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Nephrol Dial Transplant (2014) 0: 1–39. fulltext
- ↑ Moritz ML, Ayus JC. 100cc 3% sodium chloride bolus: a novel treatment for hyponatremic encephalopathy. Metab Brain Dis. 2010 Mar; 25(1): 91-6.
- ↑ The hyponatremia formulas do not work so well (Clin J Am Soc Nephrol 2007;2:1110 and Nephrol Dial Transplant 2006;21:1564)
- ↑ 9.0 9.1 9.2 Schrier RW, Bansal S. Diagnosis and management of hyponatremia in acute illness. Curr Opin Crit Care 2008;14:627-34
- ↑ Nagler EV1, Vanmassenhove J, van der Veer SN et al. Diagnosis and treatment of hyponatremia: a systematic review of clinical practice guidelines and consensus statements. BMC Med. 2014 Dec 11;12:1