We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Acute kidney injury
From WikEM
(Redirected from Renal failure)
Contents
Background
- Majority of cases of community-acquired ARF is secondary to volume depletion
RIFLE Classification
- Risk - Serum creatinine increased 1.5x baseline
- Injury - Serum creatinine increased 2.0x baseline
- Failure - Serum creatinine increased 3.0x baseline OR creatinine >4 and acute increase >0.5
- Loss - Complete loss of kidney function for >4wk
- ESRD - Need for renal replacement therapy for >3mo
Chronic Kidney Disease Stages
- Useful if patient's baseline creatinine is unknown
- Stage 1: Kidney damage (e.g. proteinuria) and normal GFR; GFR >90
- Stage 2: Kidney damage (e.g. proteinuria) and mild decrease in GFR; GFR 60-89
- Stage 3: Moderate decrease in GFR; GFR >30-59
- Stage 4: Severe decrease in GFR; GFR 15-29
- Stage 5: Kidney failure (dialysis or kidney transplant needed); GFR <15
Risk Factors
- Radiocontrast agents
- Especiallyif GFR <60, hypovolemic
- Atherosclerosis
- Chronic hypertension
- Chronic kidney disease
- NSAIDs
- ACEI/ARB
- Sepsis
- Hypercalcemia
- Hepatorenal syndrome
Clinical Features
- Acute renal failure itself has few symptoms until severe uremia develops:
- Nausea/vomiting, drowsiness, fatigue, confusion, coma
- Patients more likely to present with symptoms related to underlying cause:
- Prerenal
- Thirst, orthostatic light-headedness, decreasing urine output
- Intrinsic
- Flank pain, hematuria
- Nephrolithiasis
- Papillary necrosis
- Crystal-induced nephropathy
- Myalgias, seizures, recreational intoxication
- Pigment-induced ARF (rhabdomyolysis)
- Darkening urine and edema (esp with preceding pharyngitis or cutaneous infection)
- Acute glomerulonephritis
- Fever, arthralgia, rash
- Acute interstitial nephritis
- Cough, dyspnea, hemoptysis
- Goodpasture, granulomatosis with polyangiitis (Wegener's)
- Flank pain, hematuria
- Postrenal
- Alternating oliguria and polyuria is pathognomonic of obstruction
- Anuria
- Prerenal
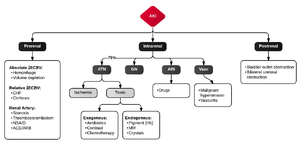
Etiologies
Prerenal
- Hypovolemia
- GI: decreased intake, vomiting and diarrhea
- Hemorrhage
- Pharmacologic: diuretics
- Third spacing
- Skin losses: fever, burns
- Miscellaneous
- Hypoaldosteronism
- Salt-losing nephropathy
- Postobstructive diuresis
- Hypotension
- Sepsis
- Decreased cardiac output
- Hepatorenal Syndrome
- Ischemia/infarction
- Valvulopathy
- Pharmacologic
- Beta-blockers
- Calcium-channel blockers
- Antihypertensive medications
- High output heart failure
- Thyrotoxicosis
- AV fistula
- Renal artery and small-vessel disease
- Embolism: thrombotic, septic, cholesterol
- Thrombosis: atherosclerosis, vasculitis, sickle cell disease
- Dissection
- Pharmacologic
- Microvascular thrombosis
- Hypercalcemia
Intrinsic
- Tubular diseases
- Ischemic acute tubular necrosis
- Caused by more advanced disease due to the prerenal causes
- Ischemic acute tubular necrosis
- Nephrotoxins
- Aminoglycosides, radiocontrast, amphotericin B, heme pigments (rhabdomyolysis, hemolysis)
- Obstruction
- Uric acid, calcium oxalate from Ethylene Glycol Toxicity, Multiple myeloma (immunoglobin light chains), amyloid
- Pharmacologic: sulfonamide, triamterene, acyclovir, indinavir
- Interstitial diseases
- Acute interstitial nephritis: typically a drug reaction (NSAIDs, Penicillins and antibiotics, Diuretics, phenytoin)
- Infection: bilateral pyelonephritis, Legionella, Hantavirus
- Infiltrative disease: sarcoidosis, lymphoma
- Autoimmune diseases: SLE
- Glomerular diseases
- Rapidly progressive glomerulonephritis
- Goodpasture, granulomatosis with polyangiitis (Wegener's) HSP, SLE, membranoproliferative GN
- Postinfectious glomerulonephritis
- Rapidly progressive glomerulonephritis
- Small-vessel diseases
- Microvascular thrombosis
- Preeclampsia, HUS, DIC, TTP, vasculitis (PAN, SCD, atheroembolism)
- Malignant hypertension
- Scleroderma
- Renal vein thrombosis
- Microvascular thrombosis
Postrenal
- Infants and children
- Urethra and bladder outlet
- Anatomic malformations
- Urethral atresia
- Meatal stenosis
- Anterior and posterior urethral valves
- Anatomic malformations
- Ureter
- Anatomic malformations
- Vesicoureteral reflux (female preponderance)
- Ureterovesical junction obstruction
- Ureterocele
- Retroperitoneal tumor
- Anatomic malformations
- Urethra and bladder outlet
- All ages
- Various locations in GU tract
- Trauma
- Blood clot
- Urethra and bladder outlet
- Phimosis or urethral stricture (male preponderance)
- Neurogenic bladder
- Diabetes mellitus, spinal cord disease, multiple sclerosis, Parkinson's
- Pharmacologic: anticholinergics, a-adrenergic antagonists, opioids
- Various locations in GU tract
- Adults
- Urethra and bladder outlet
- BPH
- Cancer of prostate, bladder, cervix, or colon
- Obstructed catheters
- Ureter
- Calculi, uric acid crystals
- Papillary necrosis
- SCD, DM, pyelonephritis
- Tumor: Ureter, uterus, prostate, bladder, colon, rectum; retroperitoneal lymphoma
- Retroperitoneal fibrosis: idiopathic, tuberculosis, sarcoidosis, propranolol
- Stricture: TB, radiation, schistosomiasis, NSAIDs
- Miscellaneous
- Aortic aneurysm
- Pregnant uterus
- IBD
- Trauma
- Urethra and bladder outlet
Evaluation
- Prerenal
- BUN/creatinine ratio > 20
- FeNa <1% ((urine sodium/plasma sodium) / (urine creatinine / serum creatinine))
- < 2% for neonates
- Urine osm >500
- Urine sodium < 20 mEq/L
- Specific gravity > 1.020
- Fractional excretion of urea < 35%
- Microscopic analysis
- Hyaline casts
- Instrinsic
- FeNa >1%
- > 2.5% for neonates
- Urine Osm <350
- Urine sodium > 40 mEq/L
- Specific gravity < 1.020
- Fractional excretion of urea > 50%
- Microscopic analysis
- Acute glomerulonephritis: RBCs, casts
- Acute tubular necrosis: protein, tubular epithelial cells
- FeNa >1%
- Postrenal
- FeNa >1%
- Urine Osm <350
Work-up
- Urine
- Prostate exam
- Urinalysis, urine sodium, urine creatinine, urine urea
- ECG (hyperkalemia)
- Chronic renal failure features
- Anemia, thrombocytopenia
- Iron studies with low Fe, low TIBC, low iron saturation, normal ferritin
- Secondary rise in PTH, high phos, low calcium
Imaging
- CXR
- Evidence of volume overload, pneumonia
- US
- Test of choice in setting of acute renal failure
- Bladder size (post-void)
- Hydronephrosis
- IVC collapsibility (prerenal)
- CT
- Useful to determine cause of post renal failure (identification of abdominal masses etc.)
- Should generally not be used with IV contrast due to potential risk for CIN
- Indicated if hydronephrois found on ultrasound in order to define the location of obstruction
Management
Treat underlying cause
- Prerenal: IVF
- Intrinsic: Depends on cause
- Obstruction:
- Note: Postobstructive diuresis can result in significant volume loss and death
- Typically occurs when obstruction has been prolonged / has resulted in renal failure
- Admit patients with persistent diuresis of >250 mL/h for >2hr
- Foley Catheter, consider Coude Catheter
- Suprapubic (if Coude fails)
- Note: Postobstructive diuresis can result in significant volume loss and death
Dialysis
- Indicated for:
- A: Acidosis (severe)
- E: Electrolyte abnormality (e.g. uncontrolled hyperkalemia)
- I: Ingestions (lithium, ASA, methanol, ethylene glycol, theophylline)
- O: Overload (volume) with persistent hypoxia
- U: Uremic pericarditis/encephalopathy/bleeding dyscrasia
- Also:
- Na <115 or >165 mEq/L
- creatinine > 10
- BUN >100
Disposition
- Admit