We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
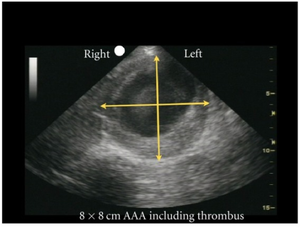
Abdominal aortic aneurysm
From WikEM
Contents
Background
- Infrarenal diameter >3cm or >50% increase in size of diameter
- 85% of cases are infrarenal [1]
- M to F ratio is 4:1
- Rupture Risk
- <4cm: low risk for rupture
- 4-5cm: 5 year risk 3-12%
- >5cm: 25-41%
- Rupture possible at any size, most commonly >5cm
- Mortality with rupture: 85-90% [1]
Risk Factors
- Smoking
- Risk factor most strongly associated with AAA
- Also promotes the rate of aneurysm growth
- Age (prevalence is negligible in age <50yrs)
- Family history
- Hypertension
- Diabetes mellitus
- Hyperlipidemia
Clinical Features
- Classic triad is pain + hypotension + pulsatile mass
- Pain often described as sudden, severe, radiating to back
- Syncope (10%)
- Signs of Retroperitoneal hemorrhage
- Massive GI bleed from erosion into intestines
- Pain + AAA = rupture until proven otherwise
- Acute abdomen + hypotension = possible rupture
- Gross Hematuria can be caused by an aortocaval fistula (very rare)
Differential Diagnosis
Diffuse Abdominal pain
- Abdominal aortic aneurysm
- Acute gastroenteritis
- Aortoenteric fisulta
- Appendicitis (early)
- Bowel obstruction
- Bowel perforation
- Gastroparesis
- Diabetic ketoacidosis
- Inflammatory bowel disease
- Mesenteric ischemia
- Pancreatitis
- Peritonitis
- Sickle cell crisis
- Spontaneous bacterial peritonitis
- Volvulus
Lower Back Pain
- Spine related
- Acute ligamentous injury
- Acute muscle strain
- Disk herniation (Sciatica)
- Degenerative joint disease
- Spondylolithesis
- Epidural compression syndromes
- Spinal fracture
- Cancer metastasis
- Spinal stenosis
- Transverse myelitis
- Vertebral osteomyelitis
- Ankylosing spondylitis
- Spondylolithesis
- Discitis
- Renal disease
- Intra-abdominal
- Abdominal aortic aneurysm
- Ulcer perforation
- Retrocecal appendicitis
- Large bowel obstruction
- Pancreatitis
- Pelvic disease
- Other
- Retroperitoneal hemorrhage/mass
- Meningitis
Evaluation
- Ultrasound
- ~100% sensitive for increased diameter
- Cannot reliably visualize rupture
- CT
- ~100% sensitive for increased diameter and rupture
- IV contrast is preferred but not essential
Management
Rupture
- Do not waste time in ED trying to "stabilize" patient
- Immediate surgery consultation/ go to OR
- Crossmatch 6 units of pRBC
- Pain control (avoid hypotension)
- Antihypertensives (use with caution, goal SBP 110-120 mmHg or MAP 70-80)[2]
- Labetalol: 20mg IV, then 40-80mg IV q10 min (max 300mg)
- Esmolol: Bolus 500 mcg/kg, then 50-200 mcg/kg/min
- Nitroprusside: 0.3 - 0.5 mcg/kg/min, titrate to max 10 mcg/kg/min
- Controversial
- Too little (ischemia), too much (increased bleeding)
- Consider allowing for permissive hypotension (SBP 80-100) in conscious patient
- Pressors
- Norepinephrine 0.05mcg/kg/min IV; titrate by 0.02mcg/kg/min q5min
- Phenylephrine 100-180mcg/min; titrate by 25mcg/min q10min
- Dopamine 5mcg/kg/min; titrate by 5mcg/kg/min q10min
- Too little (ischemia), too much (increased bleeding)
Asymptomatic
- Prompt vascular surgery outpatient follow-up appt
- Endovascular (75%) vs open repair
- Screening frequency:
- 3-4 cm diameter: 12 months
- 4-5 cm diameter: 6 months
- 5-6 cm diameter: 1 month
- Elective Surgery indicated if:
Complications
- Aortoenteric fistula
- Aortocaval fistula
- Inflammatory abdominal aortic aneurysm
- Acute limb ischemia - embolism to lower extremities
Disposition
- Admit to OR in cases of ruptured OR
- Vasc surgery follow up in asymptomatic cases