We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
FAST exam
From WikEM
(Redirected from FAST)
Contents
Background
- Prioritize: Do primary survey of ATLS first ABCDE
- FAST exam follows ABCDE to assess “C” looking for free fluid
- Sensitivity of 42% and specificity of ≥98%[1][2]
- As little as 100ml of free fluid can be seen[3][4], though >500ml is needed for the common user[5]
- If blunt trauma start with RUQ view first
- In penetrating start with cardiac views first to rule out tamponade
- Serial exams extremely helpful
Indications
- FAST is useful in patients with blunt or penetrating traumatic injury
- Enables trauma bay decision:
- Stable patient with traumatic mechanism of injury + negative FAST → observation
- Stable patient with traumatic mechanism of injury + positive FAST → CT
- Unstable patient with traumatic mechanism of injury + negative FAST → repeat FAST or CT
- Unstable patient with traumatic mechanism of injury + positive FAST → laparotomy
Technique
- Select probe
- Curvilinear/large convex probe is ideal but phased array probe may be substituted
- Location
- Sequence can vary depending on mechanism of injury
- Include cardiac, RUQ, pelvic, and LUQ views
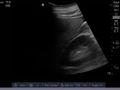
Cardiac
- Location
- Subxiphoid
- Landmarks
- Visualize the heart and pericardium using the liver as an acoustic window
- Scan anterior to posterior through the heart
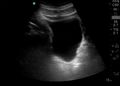
RUQ
- Location
- Coronal view over the right flank
- Landmarks
- Visualize the interface between the liver and kidney
- Scan anterior to posterior identifying Morison’s pouch and the superior and inferior pole of the kidney
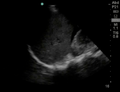
Pelvic
- Location
- Sagittal view just superior to the pubic symphysis
- Landmarks
- Identify the bladder
- Scan medial to lateral to identify fluid posterior and superior to the bladder
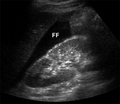
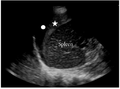
LUQ
- Location
- Coronal view over the left flank
- Landmarks
- Identify the space between the spleen and diaphragm and the spleen and the kidney
- Scan through anterior to posterior of the splenodiaphragmatic space and superior and inferior pole of the kidney
Findings
- Positive FAST will have one of the following:
- Anechoic area within the pericardial space
- Anechoic areas between the liver and kidney
- Anechoic areas between the diaphragm and spleen
- Anechoic areas between the spleen and kidney
- Anechoic areas between superior and posterior to the posterior wall of the bladder
Images
Normal
Abnormal
Pearls and Pitfalls
- Morison’s pouch
- Scans must scan through the inferior poles of the kidneys as this can contain small quantities of fluid
- Serial exam may be needed
- Negative exam does not rule out intraabdominal injuries
- Retroperitoneal hemorrhage no easily identified
- Those with delayed presentation may have clotted and not completely anechoic fluid collections
Documentation
Normal Exam
A bedside FAST ultrasound was conducted to assess for free fluid with clinical indication of trauma. Cardiac, RUQ, pelvic, and LUQ views were adequately obtained. There was no free fluid identified.
Abnormal Exam
A bedside FAST ultrasound was conducted to assess for free fluid with clinical indication of trauma. Cardiac, RUQ, pelvic, and LUQ views were adequately obtained. There was free fluid identified in the RUQ suggesting intraabdominal hemorrhage.
Clips
Normal
Abnormal
External Links
- Sonoguide: Ultrasound in Trauma – The FAST Exam
- EMCrit: Podcast 102 – Don’t Half-Ass your FAST!
- eFAST : extended Focused Assessment with Sonography in Trauma
See Also
- EFAST exam
- Cardiac ultrasound
- IVC ultrasound
- Ultrasound: Lungs
- Ultrasound (Main)
- Renal ultrasound
- Bladder ultrasound
- Abdominal Trauma
- Ultrasound: In Shock and Hypotension
References
- ↑ Natarajan B, Gupta PK, Cemaj S, et al. FAST scan: Is it worth doing in hemodynamically stable blunt trauma patients? Surgery. 2010;148(4):695-700.
- ↑ Miller MT, Pasquale MD, Bromberg WJ, et al. Not so FAST. J Trauma. 2003; 54(1):52-59.
- ↑ Goldberg GG. Evaluation of ascites by ultrasound. Radiology. 1970; 96(15):217–221.
- ↑ Von Kuenssberg Jehle D, Stiller G, Wagner D. Sensitivity in detecting free intraperitoneal fluid with the pelvic views of the FAST exam. Am J Emerg Med. 2003 Oct;21(6):476-478.
- ↑ McKenney KL, McKenney MG, Cohn SM, et al. Hemoperitoneum score helps determine need for therapeutic laparotomy. J Trauma 2001; 50(4):650–654.
.gif/120px-Subxiphoid_(Still).gif)