Deep venous thrombosis
Contents
Background

Clinical Spectrum of Venous thromboembolism
- Deep venous thrombosis (uncomplicated)
- Phlegmasia alba dolens
- Phlegmasia cerulea dolens
- Venous gangrene
- Pulmonary embolism
- Isolated distal deep venous thrombosis
Only 40% of ambulatory ED patients with PE have concomitant DVT[1][2]
Anatomy
Significant risk of PE:
- Common femoral vein
- (Superficial) femoral vein
- (Superficial) femoral vein is part of the deep system, not the superficial system as the name suggests!
- Popliteal veins
Clinical Features
Physical Exam
- Leg swelling with circumference >3cm more than unaffected side
- Tenderness over calf muscle
- Homan's sign - pain during dorsiflexion of foot (SN 60-96% and SP 20-72%)[3]
Differential Diagnosis
- Arterial thrombosis
- Cellulitis
- Septic Joint
- Osteomyelitis
- Compartment Syndrome
- Nec fasc
- Gout
- Neuropathy
- Nerve entrapment
- Sciatica
- Fracture
- Reflex Sympathetic Dystrophy
- Lymphangitis
- Buerger's disease
- Arthritis
- Tendonitis
- Myositis
- Arteritis
- Paget-Schroetter Syndrome
Calf pain
- DVT
- Compartment syndrome
- Gastrocnemius strain
- Calcaneal bursitis
- Achilles tendon rupture
- Cellulitis
- Superficial thrombophlebitis
- Ruptured Popliteal cyst (Baker's)
Evaluation
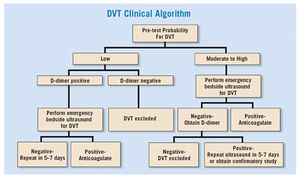
- Clinical exam
- Risk stratification for further testing indicated using, e.g. Modified Wells Score
Modified Wells Score
Can be applied for patients whose clinical presentation is concerning for a DVT in order to risk stratify.
- Active cancer (<6 mo) - 1pt
- Paralysis, paresis, or immob of extremity - 1pt
- Bedridden >3 d b/c of symptoms (within 4 wk) - 1pt
- TTP along deep venous system - 1pt
- Entire leg swollen - 1pt
- Unilateral calf swelling >3cm below tibial tuberosity - 1pt
- Unilateral pitting edema - 1pt
- Collateral superficial veins (not varicose) - 1pt
- Previously documented DVT - 1pt
- Alternative diagnosis as likely or more likely than DVT - (-)2pts
- A score of 0 or lower → minimal risk - DVT prevalence of 5%. D-dimer testing is safe in this group - negative d-dimer decreases the probability of disease to <1% allowing an ultrasound to be deferred.
- A score of 1-2 → moderate risk - DVT prevalence of 17%. D-dimer testing still effective and a negative test decreases post-test probability disease to <1%
- A score of 3 or higher → high risk - DVT prevalence of 17-53% → patients should receive an ultrasound[4]
Management
The distinction between distal and proximal relates to veins below and above the knee respectively.[5] Patients with superficial venous thromboses such as the long saphenous and short saphenous are at risk of developing a DVT, especially in patients who have a history of prior DVT although management with anticoagulation is controversial.[6]
Proximal DVT
Proximal veins are the external iliac, common femoral, greater saphenous, profound femoral, (superficial) femoral vein, popliteal vein
- If NO phlegmasia cerulea dolens:
- If phlegmasia cerulea dolens:
- If anticoagulation contraindicated:
Distal DVT
Distal veins are the anterior tibial, posterior tibial, peroneal, gastrocnemius, soleus.
- Symptomatic
- Asymptomatic with extension of thrombus toward proximal veins
- Asymptomatic without extension
- Discharge with compressive U/S q2 weeks
VTE in Pregnancy[7]
- Therapeutic LMWH or unfractionated heparin anticoagulation dose in:
- Antepartum outpatient with multiple prior VTEs or any VTE with high-risk thrombophilia until 6 weeks postpartum
- Postpartum inpatient with prior unprovoked, estrogen-provoked VTE, or low-risk thrombophilia for duration of admission
- Lower prophylactic anticoagulation dose in:
- Antepartum outpatient with prior unprovoked, estrogen-provoked VTE, or low-risk thrombophilia until6 weeks postpartum
- Patients admitted > 72 hrs, not at high risk for bleeding or imminent delivery
- Resume 12 hours after C-section and removal of epidural / spinal needle in indicated patients
- Halt anticoagulation if imminent delivery, C-section, epidural / spinal needle
Recurrent DVT on Therapeutic Anticoagulation
- Admit patients for vascular surgery and hematologist consult
- Consider Greenfield IVC filter placement
- Typically start heparin for additional anticoagulation
Anticoagulation Options
Coumadin Regimen
- Standard anticoagulation regimen
- Enoxaparin 1mg/kg q12h 4-5 days
- Coumadin
- typical starting dose 5mg/day
- give 7d supply with first dose in ED
- GFR <30 and/or potentially requiring reversal
- Unfractionated Heparin 80 units/kg bolus then 18 units/kg/hour
- Check PTT after 6hr; adjust infusion to maintain PTT at 1.5-2.5x control
- Coumadin as above
- Unfractionated Heparin 80 units/kg bolus then 18 units/kg/hour
Rivaroxaban (Xarelto) Regimen
- Standard
- Start 15mg PO BID x 21 days, then 20mg PO daily (duration depending on risk factors)
- No need for initial enoxaparin
- Renal dosing
- Check creatinine on all patients prior to initiation
- CrCl <30 avoid use
Apixaban (Eliquis) Regimen
- Standard
- Start 10mg PO BID x 7 days, then 5mg PO BID daily (duration depending on risk factors)
- No need for initial enoxaparin
- Renal dosing
- No dosage adjustments necessary for renal impairment, but CrCl <25 mL/minute were excluded from clinical trials
Contraindications to anticoagulation
- Active hemorrhage
- Platelets <50
- History of intracerebral hemorrhage
Disposition
- Consider discharge if all of the following are present:
- Admit for any of the following:
- Iliofemoral DVT
- Phlegmasia cerulea dolens
- High risk of bleeding on anticoagulation
- Significant comorbidities
- Symptoms of concurrent PE
- Recent (within 2 weeks) stroke or transient ischemic attack
- Severe renal dysfunction (GFR < 30)
- History of heparin sensitivity or Heparin-Induced Thrombocytopenia
- Weight > 150kg
See Also
External Links
References
- ↑ Righini M, Le GG, Aujesky D, et al. Diagnosis of pulmonary embolism by multidetector CT alone or combined with venous ultrasonography of the leg: a randomised non-inferiority trial. Lancet. 2008; 371(9621):1343-1352.
- ↑ Daniel KR, Jackson RE, Kline JA. Utility of the lower extremity venous ultrasound in the diagnosis and exclusion of pulmonary embolism in outpatients. Ann Emerg Med. 2000; 35(6):547-554.
- ↑ Anand SS, et al. Does this patient have deep vein thrombosis? JAMA. 1998; 279(14):1094-9.
- ↑ Del Rios M et al. Focus on: Emergency Ultrasound For Deep Vein Thrombosis. ACEP News. March 2009. https://www.acep.org/clinical---practice-management/focus-on--emergency-ultrasound-for-deep-vein-thrombosis/
- ↑ Gualtiero P. How I treat isolated distal deep vein thrombosis (IDDVT). Blood 2014 123:1802-1809; doi: https://doi.org/10.1182/blood-2013-10-512616
- ↑ Litzendorf ME. Satiani B. Superficial Venous thrombosis:disease progression and evolving treatment approaches. Vasc Health Risk Manag. 2011(7). 569-575
- ↑ DʼAlton ME et al. National Partnership for Maternal Safety: Consensus bundle on venous thromboembolism. Obstet Gynecol 2016 Oct; 128:688.

