We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Compartment syndrome
From WikEM
(Redirected from Compartment Syndrome)
Contents
Background
- Most commonly caused by tibia fracture (anterior compartment)
Compartment Syndrome Indications
- Consider whenever pain or paresthesia occurs in an extremity after:
- fracture
- crush injury
- immobilizaition
- snake bites
- burns
- prolongued tourniquet application
- fluid extravasation into a limb
- soft tissue infection
- extreme exertion
- Immediate threat is viability of nerve and muscle; later threat is infection, gangrene, Rhabdomyolysis, Renal Failure
Pathophysiology
- Tissue perfusion is difference between diastolic BP and compartment pressure
- As compartment pressure increases, tissue perfusion decreases
Etiologies
- Orthopedic
- Vascular
- Ischemic-reperfusion injury
- Hemorrhage
- Iatrogenic
- Vascular puncture in anticoagulated patients
- IV/intra-arterial drug injection
- Constrictive casts
- Soft tissue injury
- Prolonged limb compression
- Crush injury
- Burn
- Snake bite
Clinical Features
General Symptoms
- Compartment is swollen, firm, tender with squeezing
- Usually develops soon after significant trauma
- May be delayed up to 48hr after the event
5 P's
- Classic signs of disruption in arterial flow, not of compartment syndrome
- Only found once arterial flow has stopped (very late finding)
- Pain
- Severe, out of proportion to physical findings
- Worse with passive movement (muscle extension > increased volume > increased pressure)
- Often the presenting symptom.
- Paresthesia
- Occurs in sensory distribution of affected nerve
- Pallor
- Paralysis: late finding
- Pulselessness: late finding
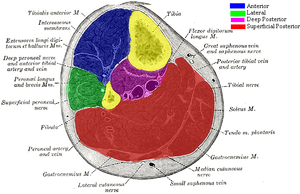
Lower Leg Specific Syndromes
- Anterior
- Nerve: deep fibular (peroneal): sensation of 1st webspace
- Muscle: tibialis anterior: foot/ankle dorsiflexion
- Lateral
- Nerve: superficial fibular (peroneal) nerve: sensation of lateral aspect of lower leg, dorsum of foot
- Muscle: peroneus longus and brevis: foot plantarflexion
- Deep posterior
- Nerve: posterior tibial nerve: sensation of plantar aspect of foot
- Muscle: tibialis posterior/flexor hallucis longus/flexor digitorum longus: Pain with passive extension of the toes
- Superficial posterior
- Nerve: sural cutaneous nerve: sensation of lateral aspect of foot
- Muscle: gastrocnemius/soleus/plantaris: weakness of plantar flexion
Hand
- Crush injury, with or with out associated fracture
- Involved compartments: thenar, hypothenar, adductor pollicis, and 4 interossei muscles
- Diagnosis
- Clinical, not based on actual compartment pressure
- Pain
- Deep, constant, poorly localized, out of proportion to exam
- "Intrinsic minus" position at rest
- MCP joint extended with proximal IP joint slightly flexed
- Pain with passive stretch of involved compartmental muscles
- Interosseus: performed with MCP joint extended and PIP jionts fully flexed
- Thenar, hypothenar: performed by extension of MCP joint
- Tense swelling of affected compartment
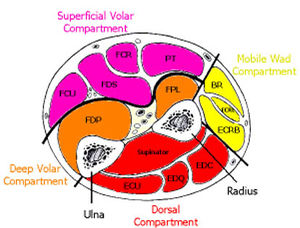
Forearm
- Associated with supracondylar fracture (peds), distal radius fracture (adults)
- Compartments
- Dorsal (highest risk)
- Volar
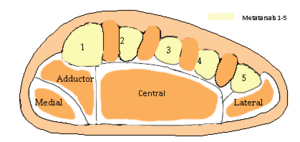
Foot
- Number of compartments is controversial, but at least 4, up to 9
- Medial, lateral, central, interosseous, adductor
- Mechanism - crush injuries
- Other mechanisms - foot surgery, Lisfranc fracture, cast immobilization, prolonged extremity positioning, snake bites, severe ankle sprains with arterial disruption[1]
- 5-17% of calcaneus fractures result in compartment syndrome
- Diagnosis
- Pain out of proprtion
- Pain worse with passive dorsiflexion (stretching intrinsic musculature of foot); concurrent metatarsal fracture cloud this finding
- Do not rely on absent pulse or complete anesthesia, which are late findings
- Measure absolute compartment pressures in insertion sites found here
- Treatment
- Elevate extremity to level of heart (above the heart, and there will be reduction of O2 perfusion)
- SCDs may help decrease interstitial pressure, improve venous return/arterial flow
- Fasciotomy within 24 hrs of injury if pressures > 30 mmHg
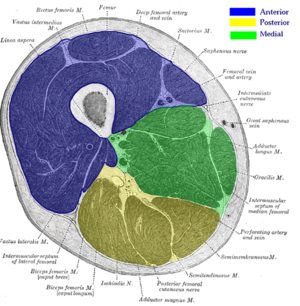
Other
- Thigh (quadriceps compartment)
- Buttock (gluteal compartment)
- Arm (deltoid, biceps compartments)
- Abdominal
Differential Diagnosis
Extremity trauma
- Peripheral nerve injury
- Vascular injury
- Tendon injury
- Laceration
- Fracture
- Open joint injury
- Crush syndrome
- Compartment syndrome
- Rhabdomyolysis
- Contusion
- Myositis ossificans
Calf pain
- DVT
- Compartment syndrome
- Gastrocnemius strain
- Calcaneal bursitis
- Achilles tendon rupture
- Cellulitis
- Superficial thrombophlebitis
- Ruptured Popliteal cyst (Baker's)
Evaluation
Work-Up
- xray to rule out fracture
- Compartment pressure (see below; take serial measurements if needed)
- Total CK, UA (rhabdomyolysis)
- Chemistry (hyperkalemia)
Measure Compartment Pressure
- Normal is <10 mm Hg
- Pressures <20 mmHg can be tolerated w/o significant damage
- Exact level of pressure elevation that causes cell death is unclear. It was previously thought pressure >30 mmHg was toxic although the "delta pressure" may be better predictor than absolute pressure
ΔPressure = [Diastolic Pressure] – [Compartment Pressure][2]
- ΔPressure < 30 mm Hg is suggestive of compartment syndrome
Management
- Fasciotomy
- Perform as soon as diagnosis is made by history/physical or by measurement
- Permanent damage results from >8hr of ischemia
- Refer here for technique: http://www.wheelessonline.com/ortho/12806
- Support blood pressure in hypotensive patient
- Place affected limb at the level of the heart or slightly dependent
- AVOID ice (will further compromise microcirculation)
- Bivalve or remove cast if present
See Also
External Links
References
- ↑ Haddad, Steven L. Managing risk: Compartment syndromes of the foot. AAOS, 2007. http://www.aaos.org/news/bulletin/janfeb07/clinical1.asp
- ↑ Elliott, KGB. Diagnosing acute compartment syndrome. J Bone Joint Surg Br. 2003 Jul;85(5):625-32. PDF