We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Cysticercosis
From WikEM
(Redirected from Taenia solium)
Contents
Background
- Parasitic infection caused by larval stage of Taenia solium (pork tapeworm)[1]
- Occurs when humans (definitive host) ingest poorly cooked pig (intermediate host) that is infected with larvae (cysticerci)
- Estimated 50-100 million people infected worldwide
- 1,000 new cases in US per year, mostly in immigrants from Latin America but also seen in those from Asia or Africa
- More than 80% of those affected are asymptomatic
- Cysts can reside anywhere in body
- Divided into extraneural cysticercosis (outside CNS) and neurocysticercosis (which can be parenchymal, extraparenchymal or both)
Clinical Features
Extraneural cysticercosis
- Subcutaneous tissue: nodules that are not cosmetically pleasing, but usually asymptomatic
- Muscle: asymptomatic or sometimes painful due to surrounding inflammation
- Cardiac cysts are rare: arrhythmias/conduction abnormalities
Neurocysticercosis (NCC)[2]
- Parenchymal NCC
- Most common presentation of NCC
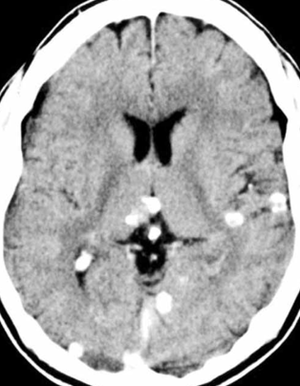
- Most cases are asymptomatic and discovered incidentally after resolution of infection (see image below)
- Those with symptoms usually present with seizures (focal or generalized)
- Focal neurologic deficit
- Extraparenchymal NCC: more often present with headaches, vomiting, hydrocephalus
- Intraventricular cysts: can get lodged in ventricular outflow tracts and cause obstructive hydrocephalus and increased ICP causing nausea, vomiting, altered mental status, papilledema
- Subarachnoid cysts: can cause inflammatory response leading to arachnoiditis which may result in hydrocephalus, meningitis, stroke, and vasculitis
- Ocular (1-3% of cases): diplopia if EOM involvement, vision loss or pain if intra-ocular
- Spinal (1% of cases): radicular pain, paresthesias, cauda equina symptoms
Differential Diagnosis
- Brain abscess
- Vasculitis
- Tuberculomas or Mycotic granulomas
- Primary brain tumors or metastases
Seizure
- Epileptic seizure
- Non-epileptic seizure
- Meningitis
- Encephalitis
- Intracranial hemorrhage
- Alcohol withdrawal
- Eclampsia
- Neurocysticercosis
- Posterior reversible encephalopathy syndrome
- Impact seizure (head trauma)
- Seizure with VP shunt
- Toxic ingestion
- Intracranial mass
- Syncope
- Hyperventilation syndrome
- Migraine headache
- Movement disorders
- Narcolepsy/cataplexy
Evaluation
Workup
- Imaging is usually best
- CT head (calcifications/edema); MRI (cysts +/- scolex, edema)[3]
- X-rays or CT for extraneural cysticercosis
- EITB assay for anticysticercal antibody
- Serum (more sensitive) or CSF studies (less common)
- Labs
- Usually not helpful
- Eosinophilia not seen unless cyst is leaking/ruptured
- Depending on presentation, involvement of the following services may be needed:
- Neurology: for seizures refractory to meds
- Neurosurgery: hydrocephalus, mass effect, herniation
- Infectious disease: if starting antiparasitic therapy
- Ophthalmology: if suspect ocular involvement or if starting antibiotics and need to confirm no ocular involvement
Evaluation
- Definitive: 1 absolute criterion, or 2 major plus 1 minor and 1 epidemiologic criteria.
- Probable: 1 major plus 2 minor criteria, or 1 major plus 1 minor plus 1 epidemiologic criteria, or 3 minor plus 1 epidemiologic criteria.
Absolute
- Demonstration of parasite from biopsy
- Cystic lesion with scolex on neuroimaging
- Direct visualization of parasites on fundoscopic exam
Major
- Lesions highly suggestive of neurocysticercosis on imaging
- Positive ELISA for anticysticercal antibodies
- Resolution of intracranial lesions after antihelminthic therapy
- Spontaneous resolution of single enhancing lesions
Minor
- Lesions compatible with neurocysticercosis on imaging
- Clinical symptoms suggestive of neurocysticercosis
- Positive ELISA for antibodies in CSF
- Cysticercosis outside of the nervous system
Epidemiologic
- Recent travel to endemic area
- Residence in endemic area
- Household contact with Taenia solium infection
Management
Asymptomatic
- Observation
Subcutaneous or intramuscular
- Typically observation
- If just one lesion or cosmetic issue, surgical excision
- Otherwise: NSAIDs
Symptomatic Neurocysticercosis
- Anticonvulsants (keppra, dilantin, newer agents)
- Antihelminthic therapy and steroids
- Treat if edema, mass effect, or vasculitis
- Don’t treat if old calcifications on CT without edema
- Before starting these meds, need to check for:
- positive PPD
- co-infection with strongyloides (steroids can cause to disseminate)
- ocular involvement (inflammation associated with dying organisms can result in vision loss by causing chorioretinitis, retinal detachment, or vasculitis)
- Patients started on therapy get admitted to watch for any adverse events initially
Ocular
- Intra-ocular: surgery [4]
- Extra-ocular muscle involvement: albendazole and steroids[5]
- Spinal intramedullary: possibly surgery
Antiparasitic Treatment
If hydrocephalus is present, CSF diversion with ventriculostomy or VP shunt by Neurosurgery and/or surgical resection of cysts is recommended rather than antiparastic treatment
Albendazole
- 15mg/kg/day divided in 2 doses[6]
- First line therapy
Praziquantel
- Second line therapy
- 50-100mg/kg/day divided in 3 doses [7]
Steroids
- Prednisone 1mg/kg/day (60mg max) or dexamethasone 0.1mg/kg/day (10mg max)
Disposition
- Home if asymptomatic or no complications with good pain control
- Admit if starting antihelminthic therapy for further testing as listed above and to monitor initial side effects of drug therapy
- ICU for uncontrolled seizures, altered mental status, increased ICP
See Also
References
- ↑ CDC Cysticercosis http://www.cdc.gov/parasites/cysticercosis/
- ↑ Wallin MT. et al. Neurocysticercosis in the United States: review of an important emerging infection. Neurology. Nov 9 2004;63(9):1559-64
- ↑ García HH, Del Brutto OH. Imaging findings in neurocysticercosis. Acta Trop. 2003;87(1):71-8
- ↑ Sharma T. et al. Intraocular cysticercosis: clinical characteristics and visual outcome after vitreoretinal surgery. Ophthalmology. 2003;110(5):996-1004
- ↑ Sundaram PM, Jayakumar N, Noronha V. Extraocular muscle cysticercosis - a clinical challenge to the ophthalmologists. Orbit. Dec 2004;23(4):255-62
- ↑ Garcia HH, Pretell EJ, Gilman RH, et al. A trial of antiparasitic treatment to reduce the rate of seizures due to cerebral cysticercosis. N Engl J Med. 2004;350(3):249-58.
- ↑ Sotelo J. et al. Albendazole vs praziquantel for therapy for neurocysticercosis. A controlled trial. Arch Neurol. May 1988;45(5):532-4