Antibiotic Resistance and Food Safety
 While many foodborne infections are mild and do not require treatment, antibiotics can be lifesaving in severe cases. Antibiotic resistance compromises our ability to treat these infections and is a serious threat to public health.
While many foodborne infections are mild and do not require treatment, antibiotics can be lifesaving in severe cases. Antibiotic resistance compromises our ability to treat these infections and is a serious threat to public health.
Salmonella and Campylobacter, two of the many bacteria commonly transmitted through food, cause an estimated 410,000 antibiotic-resistant infections in the United States each year.1
This webpage provides an overview of antibiotic resistance, how it connects to food safety, and what you can do to protect yourself and others from foodborne illness.
Antibiotic Resistance
Fast Facts
- Antibiotics are among the most commonly prescribed drugs used in human medicine.
- Antibiotic resistance is spread through the resistant strains of bacteria from person to person, or from the natural environment, including the foods we eat.
- The germs that contaminate food can be resistant because of the use of antibiotics in people and in food animals.
Antibiotics are powerful tools for fighting illness and disease, but overuse has helped create bacteria that are outliving the drugs used to treat them.
Antibiotic resistance is the ability of microbes (bacteria, viruses, fungi and parasites) to resist the effects of drugs. That means germs are not killed and their growth is not stopped.
The use of antibiotics is the single most important factor leading to antibiotic resistance around the world. Resistant bacteria are more common in settings where antibiotics are frequently used: healthcare settings, the community, and food animal production.
Efforts to prevent resistant infections include immunization, infection control, antibiotic stewardship (meaning good antibiotic prescribing practices), reducing spread from one person to another, and protecting the food supply. Learn more at the CDC's Antibiotic / Antimicrobial Resistance web site.
Can This Affect Me?
Yes. Anyone can become infected with antibiotic-resistant bacteria. In the United States, at least 2 million people become infected with bacteria that are resistant to antibiotics and at least 23,000 people die annually as a direct result of these infections1.
Although some people are at greater risk than others, no one can completely avoid the risk of antibiotic-resistant infections. Infections with resistant organisms can be difficult to treat, requiring costly and sometimes toxic alternatives. Some resistant infections cause severe illness and may result in increased recovery time, increased medical expenses, or death.
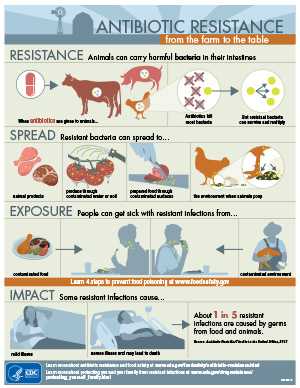
Antibiotic Resistance from the Farm to the Table
Use of antibiotics on the farm helps to produce antibiotic–resistant germs. All animals carry bacteria in their intestines. Giving antibiotics to animals will kill most bacteria, but resistant bacteria can survive and multiply.
When food animals are slaughtered and processed, these bacteria can contaminate the meat or other animal products. These bacteria can also get into the environment and may spread to fruits, vegetables or other produce that is irrigated with contaminated water. People can get exposed to resistant bacteria from animals when they:
- Handle or eat meat or produce contaminated with resistant bacteria; or
- Come into contact with animal poop
Food can get contaminated whether the bacteria are resistant to antibiotics or not. Some resistant bacteria are transmitted to people through foods.
This is important because antibiotic resistant infections from common foodborne germs, such as Salmonella, can cause more severe health outcomes than infections that are not resistant to antibiotics2.
What Can You Do?
- Take antibiotics only when needed.
- Understand the importance and seriousness of antibiotic-resistant infections linked to contaminated food.
- Know who is most at risk for infection: Young children, pregnant women, older adults, and people with weakened immune systems.
- Follow simple Food Safety Tips:
-
 CLEAN. Wash your hands and surfaces often. Germs can survive in many places around your kitchen, including your hands, utensils, and cutting boards. Wash your hands with soap after contact with animals, or animal environments. Learn more by visiting FoodSafety.gov's Clean web page.
CLEAN. Wash your hands and surfaces often. Germs can survive in many places around your kitchen, including your hands, utensils, and cutting boards. Wash your hands with soap after contact with animals, or animal environments. Learn more by visiting FoodSafety.gov's Clean web page. -
 SEPARATE. Don't cross-contaminate. Even after you've cleaned your hands and surfaces thoroughly, raw meat, poultry, seafood, and eggs can still spread germs to produce and ready-to-eat foods—unless you keep them separate. Learn more by visiting FoodSafety.gov's Separate web page.
SEPARATE. Don't cross-contaminate. Even after you've cleaned your hands and surfaces thoroughly, raw meat, poultry, seafood, and eggs can still spread germs to produce and ready-to-eat foods—unless you keep them separate. Learn more by visiting FoodSafety.gov's Separate web page. -
 COOK. Cook to the right temperature. While many people think they can tell when food is "done" simply by checking its color and texture, there's no way to be sure it's safe without following a few important, but simple steps. Use a food thermometer to ensure that foods are cooked to a safe internal temperature: 145°F for whole meats (allowing the meat to rest for 3 minutes before carving or consuming), 160°F for ground meats, and 165°F for all poultry. Learn more by visiting FoodSafety.gov's Cooks web page.
COOK. Cook to the right temperature. While many people think they can tell when food is "done" simply by checking its color and texture, there's no way to be sure it's safe without following a few important, but simple steps. Use a food thermometer to ensure that foods are cooked to a safe internal temperature: 145°F for whole meats (allowing the meat to rest for 3 minutes before carving or consuming), 160°F for ground meats, and 165°F for all poultry. Learn more by visiting FoodSafety.gov's Cooks web page. -
 CHILL. Keep your refrigerator below 40°F and refrigerate foods properly. Germs can grow in many foods within 2 hours unless you refrigerate them. (During the summer heat, cut that time down to 1 hour.) Learn more by visiting FoodSafety.gov's Chill web page.
CHILL. Keep your refrigerator below 40°F and refrigerate foods properly. Germs can grow in many foods within 2 hours unless you refrigerate them. (During the summer heat, cut that time down to 1 hour.) Learn more by visiting FoodSafety.gov's Chill web page.
- Report suspected outbreaks of illness from food to your local health department.
- Don’t prepare food for others if you have diarrhea or vomiting. Be especially careful preparing food for children, pregnant women, those in poor health, and older adults.
- Review CDC’s Traveler’s Health recommendations when preparing to travel.
Learn More
Preventing the spread of foodborne infections from resistant bacteria is not easy. The CDC works closely with a number of partners to address this important issue, including federal agencies, state and local health departments, the food industry, healthcare providers, and academia.
You can learn more about Antibiotic Resistance and Food Safety from the following resources:
- Antibiotic Resistance and Food Animals
- NARMS - Tracking Trends in Resistance
- Medscape: Clinical Impact of Antibiotic-Resistant Salmonella
- FDA's Strategy on Antimicrobial Resistance
- CDC Feature: Be Food Safe: Protect Yourself from Food Poisoning
You can learn more about Antibiotics and Healthcare from the following resources:
References
- CDC. Antibiotic Resistance Threats in the United States, 2013. Atlanta, GA: U.S Department of Health and Human Services, CDC. 2013; p.7, 36-7.
- Krueger AL, Greene SA, Barzilay EJ, et. al. Clinical outcomes of nalidixic acid, ceftriaxone, and multidrug resistant nontyphoidal Salmonella infections compared with pansusceptible infections in FoodNet sites, 2006-2008. Foodborne Pathog Dis. 2014; 11(5): 335-41.
- Page last reviewed: October 28, 2015
- Page last updated: January 12, 2016
- Content source:


 ShareCompartir
ShareCompartir