Clostridium perfringens
Clostridium perfringens is one of the most common types of foodborne illness in the United States. CDC estimates it causes nearly 1 million cases of foodborne illness each year.
Questions and Answers
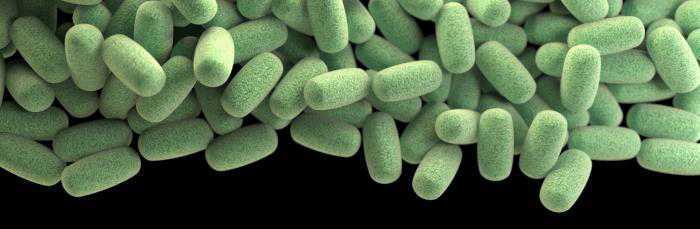
What is C. perfringens?
Clostridium perfringens (C. perfringens) is a spore-forming gram-positive bacterium that is found in many environmental sources as well as in the intestines of humans and animals. C. perfringens is commonly found on raw meat and poultry. It prefers to grow in conditions with very little or no oxygen, and under ideal conditions can multiply very rapidly. Some strains of C. perfringens produce a toxin in the intestine that causes illness.
What are common food sources of C. perfringens?
Beef, poultry, gravies, and dried or pre-cooked foods are common sources of C. perfringens infections. C. perfringens infection often occurs when foods are prepared in large quantities and kept warm for a long time before serving. Outbreaks often happen in institutions, such as hospitals, school cafeterias, prisons, and nursing homes, or at events with catered food.
What are the symptoms of C. perfringens food poisoning?
People infected with C. perfringens develop diarrhea and abdominal cramps within 6 to 24 hours (typically 8 to 12 hours). The illness usually begins suddenly and lasts for less than 24 hours. People infected with C. perfringens usually do not have fever or vomiting. The illness is not passed from one person to another.
Who is at risk of C. perfringens food poisoning?
Everyone is susceptible to food poisoning from C. perfringens. The very young and elderly are most at risk of C. perfringens infection and can experience more severe symptoms that may last for 1 to 2 weeks. Complications, including dehydration, may occur in severe cases.
How is C. perfringens diagnosed and treated?
Laboratories diagnose C. perfringens food poisoning by detecting a type of bacterial toxin in feces or by tests to determine the number of bacteria in the feces. A count of at least 106 C. perfringens spores per gram of stool within 48 hours of when illness began is required to diagnose infection. Oral rehydration or, in severe cases, intravenous fluids and electrolyte replacement can be used to prevent or treat dehydration. Antibiotics are not recommended.
What causes C. perfringens food poisoning?
Although C. perfringens may live normally in the human intestine, illness is caused by eating food contaminated with large numbers of C. perfringens bacteria that produce enough toxin in the intestines to cause illness.
C. perfringens can survive high temperatures. During cooling and holding of food at temperatures from 54°F–140°F (12°C–60°C), the bacteria grows. It can grow very rapidly between 109°F–117°F (43°C–47°C). If the food is served without reheating to kill the bacteria, live bacteria may be eaten. The bacteria produce a toxin inside the intestine that causes illness.
Prevention Tips

- Cook and keep food at the correct temperature
Food, especially roasts of beef or poultry, should be cooked to a safe internal temperature, and then kept at 140°F (60°C) or warmer or 40°F (4.4°C) or cooler. These temperatures prevent the growth of C. perfringens spores that might have survived cooking. Meat dishes should be served hot, within 2 hours after cooking.
- Refrigerate leftovers and reheat them properly

Leftover foods should be refrigerated at 40°F or colder as soon as possible and within 2 hours of preparation. It is OK to put hot foods directly into the refrigerator. However, large amounts of food, such as soups, stews, and big cuts of meats, such as roasts, should be divided into small quantities for refrigeration. Leftovers should be reheated to at least 165°F (74°C) before serving.
- When in doubt, throw it out
Foods that have dangerous bacteria in them may not taste, smell, or look different. Any food that has been left out too long may be dangerous to eat, even if it looks OK.
More Information
- CDC Feature: Tips to Prevent Illness from Clostridium Perfringens
- CDC Feature: Food Safety for Your Holiday Turkey
- Epidemiology of Foodborne Disease Outbreaks Caused by Clostridium perfringens, United States, 1998-2010.
- Foodsafety.gov: Safe Minimum Cooking Temperatures
- Foodsafety.gov: Clean, Separate, Cook, and Chill Guidelines
- USDA: Let’s Talk Turkey: A Consumer Guide to Safely Thawing and Roasting a Turkey
- USDA: Turkey Basics: Safe Cooking
- USDA: Tips for Cooking Turkeys When You’re Not Using a Conventional Oven
- CDC: Foodborne Germs and Illnesses
Publications
- Scallan E, Hoekstra RM, Mahon BE, Jones TF, Griffin PM. An assessment of the human health impact of seven leading foodborne pathogens in the United States using disability adjusted life years. Epidemiol Infect. 2015 Oct;143(13):2795–804. PubMed DOI
- Bennett SD, Walsh KA, Gould LH. Foodborne disease outbreaks caused by Bacillus cereus, Clostridium perfringens, and Staphylococcus aureus—United States, 1998–2008. Clin Infect Dis. 2013 Aug; 57(3):425–33. PubMed DOI
- Grass JE, Gould LH, Mahon BE. Epidemiology of foodborne disease outbreaks caused by Clostridium perfringens, United States, 1998–2010. Foodborne Pathog Dis. 2013 Feb; 10(2):131–6. PubMed DOI
- Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, et al., Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis, 2011 Jan. 17(1): 7–15. PubMed DOI
- Page last reviewed: January 10, 2017
- Page last updated: January 10, 2017
- Content source:


 ShareCompartir
ShareCompartir