Interim Guidance for a Health Response to Contain Novel or Targeted Multidrug-resistant Organisms (MDROs)

This document is intended for state and local health departments and healthcare facilities and serves as general or resistance mechanisms. It is not intended to describe all the actions that might be required for control of an outbreak (e.g., sustained transmission within a facility or region). In addition, further evaluation might be required based on the findings of the initial response described in this document.
Print version: Interim Guidance for a Health Response to Contain Novel or Targeted MDROs [PDF – 10 pages]
General Recommendations
Pathogen-specific guidance for some MDROs can be found here:
Healthcare facilities and laboratories should contact state or local public health authorities in a timely manner when targeted resistant organisms (e.g., pan-resistant organism) or mechanisms are identified (e.g., mcr-1 producing Enterobacteriaceae).
Health departments should be aware of the expanded capacity for antimicrobial resistance-related laboratory testing through the Antimicrobial Resistance Laboratory Network (e.g., screening cultures). When testing is indicated, health departments should contact the laboratory for their region directly to discuss the availability of specific testing and to coordinate specimen submission.
Health Departments conducting these investigations may consult with CDC by contacting the healthcare outbreak duty officer at haioutbreak@cdc.gov.
Goals of prompt response and containment should include:
- Identifying if transmission/dissemination is occurring
- Identifying affected patients
- Ensuring appropriate control measures are promptly initiated/implemented to contain potential spread
- Characterizing the organism or mechanism in order to guide further response actions, patient management, and future responses
Response Tiers
The following describes three different categories of organism (Tiers 1-3) and the recommended approach to each. General definitions of each Tier are included below; however, the organisms included in each Tier may vary by region depending on the local epidemiology.
Tier 1 organisms:
Organisms in this group include those with resistance mechanisms novel to the United States (i.e., never previously or only very rarely identified in the United States) or organisms for which no current treatment options exist (pan-resistant) and that have the potential to spread more widely within a region. This category also includes organisms and resistance mechanisms for which reports and therefore experience in the United States is extremely limited and a more extensive evaluation might better define the risk for transmission. Examples of organisms in this category include vancomycin-resistant Staphylococcus aureus (VRSA).
Tier 2 organisms:
Organisms in this group include MDROs primarily found in healthcare settings but not believed to be found regularly in the region; these organisms might have been found more commonly in other areas in the United States. For these organisms information is available about how transmission occurs and the groups primarily at risk. Examples include carbapenem-resistant Enterobacteriaceae with novel mechanisms (e.g., New Delhi Metallo-β-lactamase), carbapenemase-producing Pseudomonas spp.
Tier 3 organisms:
Organisms in this group include MDROs targeted by the facility/region that are already established in the United States and have been identified before in the region but are not thought to be endemic; information is available about transmission. Examples include carbapenem-resistant Enterobacteriaceae producing Klebsiella pneumoniae carbapenemase in regions where these organisms are more regularly identified; if only rarely identified in the region, these should be considered Tier 2 organisms.
Response Recommendations by Tier
The components of the initial response will vary depending on the organism involved; click to expand each window below for recommendations for the expected response, containment and control for each group.
Tier 1 organisms:
Organisms in this group include those with resistance mechanisms novel to the United States (i.e., never previously or only very rarely identified in the United States) or organisms for which no current treatment options exist (pan-resistant) and that have the potential to spread more widely within a region. This category also includes organisms and resistance mechanisms for which reports and therefore experience in the United States is extremely limited and a more extensive evaluation might better define the risk for transmission. Examples of organisms in this category include vancomycin-resistant Staphylococcus aureus (VRSA).
Strategies:
-
Upon identification of the organism or mechanism in a laboratory, the laboratory or healthcare facility should:
- Promptly notify the patient’s primary caregiver, patient care personnel, other healthcare staff per facility policies/procedures. Generally, local and state public health departments, and federal public health authorities should also be notified.
- Ensure timely implementation of appropriate infection control measures.
- Inform patient and family.
- If more than one month has passed since the initial culture was collected, retesting of the index patient to determine if the patient is still colonized and/or infected should be conducted if required to inform infection control precautions or to guide the subsequent investigation. Body sites for specimen collection will depend on the organism. For example:
- Staphylococci might require cultures of nares, axillae, groin, pharynx; Enterobacteriaceae might require cultures of wounds, stool, and the groin; Non-fermenting Gram-negative bacilli might require cultures of wounds, stool, sputum, and the groin.
- Testing of the site that was initially positive is usually indicated particularly if the initial site was a wound or urine.
- Periodic testing (e.g., monthly) of the index patient and/or others found to be colonized will be needed to inform the duration of control measures. In general, two or more negative results obtained at least several days apart while off of antibiotic therapy (for at least one week) that would be expected to be active against the organism should be obtained before colonization is considered resolved and a change in infection control precautions is considered. Note that decisions to discharge the patient from one level of care to another should be based on clinical criteria and not on the period of colonization.
-
Conduct a healthcare investigation.
- Review the patient’s healthcare exposures prior to and after the initial positive culture, including overnight stays in healthcare settings, outpatient visits, and home health visits. In general, healthcare exposures over the preceding month should be investigated unless information is available about the time that the organism was most likely acquired.
-
Conduct a contact investigation.
- Obtain specimens from the contacts of patients infected or colonized with target MDROs. In general, contacts should be categorized based on their level of interaction with the index patient. In general, the recommendations below may apply to healthcare exposures the index-patient had within the month prior to the identification of the target organism unless information is available about the likely time of acquisition.
- Depending on the extent of recent inpatient healthcare exposure, screening cultures of epidemiologically-linked patients should be performed; at a minimum this should include roommates. Roommates should be identified and cultured even if they have been discharged from the facility.
- If the index patient was not on Contact Precautions during their entire stay in a healthcare facility, then additional screening is recommended. Surveys could initially be limited to the contacts at highest risk for acquisition including those who overlapped with the patient for 3 or more days and who have a risk factor for MDRO acquisition (e.g., being bedbound or requiring higher levels of care, being on antibiotics, or being on mechanical ventilation). Alternatively, facilities may choose to screen entire units with point prevalence surveys.
- For many Tier 1 organisms, if the index patient was on Contact Precautions during their entire stay and adherence is high, then screening contacts beyond roommates is generally not recommended but could be considered in specific instances when the index-patient is believed to be high-risk for transmission (e.g., bed bound, on antibiotics, incontinent of stool for enteric organisms). However, if the MDRO is a novel organism for which data on the frequency and modes on transmission are not known, then broader screening of contacts is recommended. As above, additional screening could initially be limited to the contacts at highest risk for acquisition including those who overlapped with the patient for 3 or more days and who have a risk factor for MDRO acquisition including being bedbound or requiring higher levels of care, being on antibiotics, or being on mechanical ventilation.
- Wider surveys are clearly indicated if there is evidence or suspicion of ongoing transmission (e.g., isolates from multiple patients) or if initial screening of high-risk patients identifies transmission.
- Cultures of outpatients who were seen in the same clinic as the index patient are generally not recommended unless contact was extensive or if patients were exposed to common devices (e.g., whirlpools, etc.) and cleaning of the devices may not have been adequate.
- Cultures of healthcare personnel (HCP) with extensive index patient contact should be performed if epidemiology suggests that the organism may have spread to patients from colonized or infected HCP or from colonized or infected patients to HCP. For novel MDROs for which the risk of HCP colonization following contact with a colonized or infected patient is not known, then cultures of HCP should be considered.
- Home health workers that were physically caring for the patient for extended periods of time at home should also be considered among the potential HCP contacts.
- Prior to performing cultures of HCP, decisions should be made about how colonized or infected HCP will be managed (e.g., work restrictions).
- For organisms with a risk for transmission outside of healthcare settings (e.g., VRSA, mcr-1-producing Enteorbactericeae)or for which the risk of transmission outside of healthcare is not known, close household contacts (e.g., contacts who help care for the index patient or share a bed or bathroom with the patient) should also be screened. Similarly, family and friends who do not reside with the index patient but were physically caring for the patient for extended periods of time should be screened.
- Screening of additional household contacts should also be performed if specific actions might be implemented for those found to be colonized. For example, if household contacts have health issues that might result in admission to a healthcare facility in the near future, screening results might influence the type of transmission-based precautions used at admission.
- If household contacts are HCP, decisions about screening should consider the actions that will be taken if the contact is found to be colonized.
- Some situations may warrant screening in other non-healthcare settings (e.g., resistant organism from a young child who attends daycare).
- Clinical laboratories that performed cultures from healthcare settings that the index patient has been exposed to in the past 3 months should be targeted for prospective surveillance in order to identify organisms with similar resistance patterns from clinical cultures. Those isolates should be saved and sent for additional testing to determine if they match the organism of interest.
- Retrospective review of results from these clinical laboratories to identify organisms with similar resistance patterns should also be performed. If available, these retrospective isolates should also be tested to see if they match the organism of interest.
- The threshold to do environmental cultures should generally be lower for these organisms; however, they should primarily be reserved for:
- Organisms with a known persistence in the environment (e.g., Acinetobacter spp.) and transmission is identified or suspected.
- Situations in which questions about the extent of environmental contamination of an organism or the effectiveness of terminal cleaning exist.
-
Implement a system to ensure adherence to Infection control measures.
- Educate and inform the appropriate HCP and visitors to index patient about the organism and precautions indicated.
- Ensure adequate supplies are available to implement precautions.
- Monitor adherence to infection control practices at facilities that are caring for index patients and address gaps.
- Facilities that might care for the patient (e.g., acute care hospitals if patient is outpatient) should be notified so that they can “flag” the patient’s record so that in case of admission appropriate infection control precautions will be put into place.
- Ensure that the patient’s status and required infection control precautions are communicated at transfer.
- If the MDRO was present on admission, notification of the transferring facility should occur so appropriate review can occur at that facility.
Tier 2 organisms:
Organisms in this group include MDROs primarily found in healthcare settings but not believed to be found regularly in the region; these organisms might be found more commonly in other areas in the United States. For these organisms information is available about how transmission occurs and the groups primarily at risk. Examples include carbapenem-resistant Enterobacteriaceae with novel mechanisms (e.g., New Delhi Metallo-β-lactamase), carbapenemase-producing Pseudomonas spp.
Strategies:
-
Upon identification of the organism or mechanism in a laboratory, the laboratory or healthcare facility should:
- Promptly notify the patient’s primary caregiver, patient-care personnel, other healthcare staff per facility policies/procedures; local and state public health departments should be notified as required.
- Ensure implementation of appropriate infection control measures.
- Inform patient and family.
- Screening cultures of the index-patient should be performed to determine if the patient is still colonized if this might impact the patient’s care or the types of precautions used and more than a month has passed since the initial culture was collected. Sites will depend on organism (see above).
-
Conduct a healthcare investigation.
- Review the patient’s healthcare exposures prior to and after the positive culture including overnight stays in healthcare settings, and home health visits. In general, healthcare exposures over the preceding month should be investigated unless information is available about the time that the organism was most likely acquired.
-
Conduct a contact investigation.
- In general, the recommendations below may apply to healthcare exposures the index-patient had within the month prior to the identification of the target organism unless information is available about the likely time of acquisition.
- Depending on the extent of recent inpatient healthcare exposure, cultures of epidemiologically-linked patients; should be performed; at a minimum this should include roommates. Roommates should be identified and cultured even if they have been discharged from the facility.
- If the index-patient was not on Contact Precautions during their entire stay in a healthcare facility, then additional screening is recommended particularly in settings with longer lengths of stay (e.g., long-term acute care). Surveys could initially be limited to the contacts at highest risk for acquisition including those who overlapped with the patient for 3 or more days and who have a risk factor for MDRO acquisition (e.g., being bedbound or requiring higher levels of care, being on antibiotics, or being on mechanical ventilation). Alternatively, facilities may choose to screen entire units with point prevalence surveys.
- If the index patient was on Contact Precautions during their entire stay and adherence is high, then screening contacts beyond roommates is generally not recommended but could be considered in specific instances when the index-patient is believed to be high-risk for transmission (e.g., bed bound, on antibiotics, incontinent of stool for enteric organisms).
- Wider surveys are clearly indicated if there is evidence or suspicion of ongoing transmission (e.g., isolates from multiple patients) or if initial screening of high-risk patients identifies transmission.
- Cultures of outpatients who were seen in the same clinic as the index patient are generally not recommended unless contact was extensive or if patients were exposed to common devices (e.g., whirlpools, etc.) and cleaning of the devices may not have been adequate.
- In the absence of known or suspected transmission from HCP or other strong epidemiologic link, HCP should not be screened.
- In the absence of other epidemiologic data suggesting involvement, household contacts generally should not be screened. Household contacts who have frequent inpatient healthcare exposure could be screened if they have had extensive contact with the index patient to determine the level of precautions required at admission.
- Laboratories that have performed cultures from healthcare settings that the index patient was exposed to in recent past should be targeted for prospective surveillance in order to identify organisms with similar resistance patterns. These isolates should be saved and sent for testing to determine if they match the organism of interest.
- Retrospective review of the results from these clinical laboratories to identify organisms with similar resistance patterns should also be performed. If available, these retrospective isolates should also be tested to see if they match the organism of interest.
- Environmental cultures in these situations are generally not recommended unless transmission is identified or suspected. They could be considered if questions about the effectiveness of terminal cleaning exist.
-
Implement a system to ensure adherence to infection control measures
- Educate and inform the appropriate healthcare personnel and visitors to index patient about the organism and precautions indicated.
- Ensure adequate supplies are available to implement precautions.
- Monitor adherence to infection control practices at facilities that are caring for index patients and address gaps.
- Facilities that might care for the patient (e.g., acute care hospitals if patient is outpatient) should be notified so that they can “flag” the patient’s record so that in case of admission appropriate infection control precautions will be put into place.
- Ensure that the patient’s status and required infection control precautions are communicated at transfer.
- If the MDRO was present on admission, notification of the transferring facility should occur so appropriate review can occur at that facility.
Tier 3 organisms:
Organisms in this group include MDROs targeted by the facility/region that are already established in the United States and have been identified before in the region but are not thought to be endemic; information is available about transmission. Examples include carbapenem-resistant Enterobacteriaceae producing Klebsiella pneumoniae carbapenemase in regions where these organisms are more regularly identified; if only rarely identified in the region, these should be considered Tier 2 organisms.
Strategies:
-
Upon identification of the organism or mechanism in a laboratory, the laboratory or healthcare facility should:
- Promptly notify the patient’s primary caregiver, patient-care personnel, other healthcare staff. Per facility policies/procedures; local and state public health departments may have reporting requirements for these organisms.
- Ensure implementation of appropriate infection control measures.
- Inform patient and family.
-
Conduct a healthcare investigation
- Review the patient’s healthcare exposures prior to and after the positive culture including overnight stays in healthcare settings should be completed. Investigations for Tier 3 organisms are generally limited to the current and potentially prior admission.
-
Conduct a contact investigation
- If the patient is currently an inpatient or was recently discharged screening should be performed of roommates.
- If the index-patient was not on Contact Precautions during their entire stay in a healthcare facility, then additional screening of high risk contacts could be considered if the index-patient is high-risk for serving as a source of transmission (e.g., bed bound, on antibiotics). Surveys could initially be limited to the contacts at highest risk for acquisition including those who overlapped with the patient for 3 or more days and who have a risk factor for MDRO acquisition (e.g., being bedbound or requiring higher levels of care, being on antibiotics, or being on mechanical ventilation).
- If the index patient was on Contact Precautions during their entire stay and adherence is high, then screening contacts beyond roommates is not recommended.
- Wider screening should be done if there is evidence or suspicion of transmission (e.g., isolates from multiple patients).
- In the absence of a transmission event, screening HCP is not recommended.
- Screening household contacts is generally not recommended for Tier 3 organisms; however, household contacts who have frequent inpatient healthcare exposure could be screened if they have had extensive contact with the index patient to determine the level of precautions required at admission.
- Laboratories that perform cultures from healthcare settings that the index patient was exposed to in the recent past should be targeted for prospective surveillance in order to identify organisms with similar resistance patterns. These isolates should be saved and sent for testing to determine if they match the organism of interest.
- Retrospective review of the results from these clinical laboratories to identify organisms with similar resistance patterns should be performed. If available, these retrospective isolates could also be tested to see if they match the organism of interest.
- In the absence of transmission, environmental cultures in these situations are generally not recommended.
- If the patient is currently an inpatient or was recently discharged screening should be performed of roommates.
-
Implement a system to ensure adherence to infection control measures.
- Educate and inform the appropriate healthcare personnel and visitors to index patient about the organism and precautions indicated.
- Ensure adequate supplies are available to implement precautions.
- Monitor adherence to infection control practices at facilities that are caring for index patients and address gaps.
- Facilities that might care for the patient (e.g., acute care hospitals if patient is outpatient) should be notified so that they can “flag” the patient’s record so that in case of admission appropriate infection control precautions will be put into place.
- Ensure that the patient’s status and required infection control precautions are communicated at transfer.
- If the MDRO was present on admission, notification of the transferring facility should occur so appropriate review can occur at that facility.
Figure 1: Approach to screening healthcare contacts following identification of novel or targeted multidrug-resistant organisms
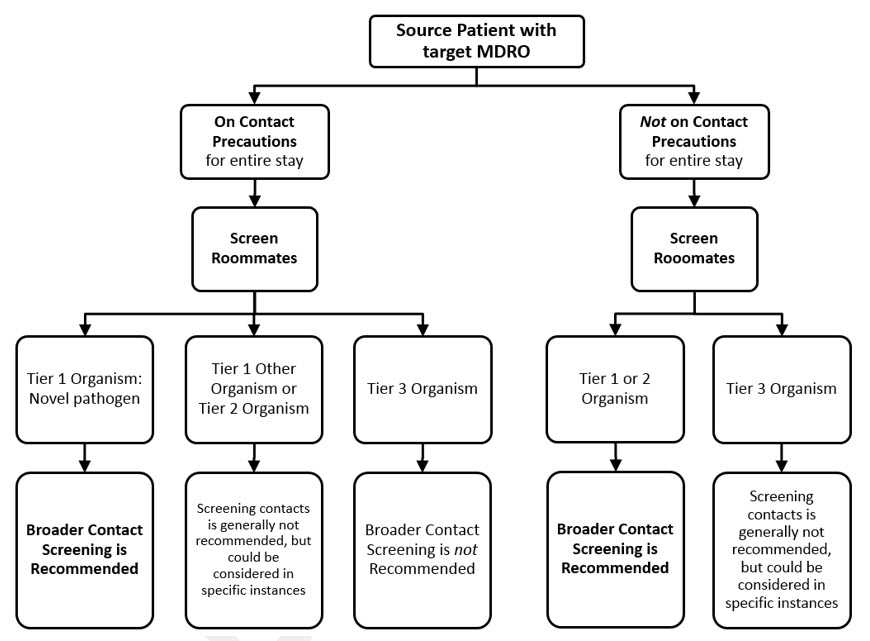
Note:
- If Contact Precautions are ordered but are not being adhered to regularly, consider the patient as not on Contact Precautions
- If more than one new patient identified with the same mechanism, more widespread screening should be conducted
- Page last reviewed: September 7, 2017
- Page last updated: September 7, 2017
- Content source:


 ShareCompartir
ShareCompartir