Surveillance
Rates of meningococcal disease are at historic lows in the United States. Tracking for meningococcal disease is very good in the United States. Health departments respond to every case of meningococcal disease and implement control measures to reduce spread of the disease.
Disease Trends
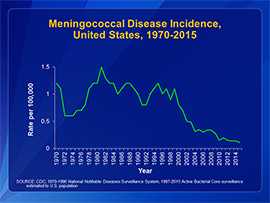
Rates of meningococcal disease have been declining in the United States since the late 1990s. In 2015, there were about 375 total cases of meningococcal disease reported. Meningococcal disease is also seasonal: the number of cases generally peaks each year in January, February, and March.
Call for Cases
Meningococcal Disease Among Men who have Sex with Men (MSM)
Download the case report form [1 page].
Meningococcal Disease Among People taking Eculizumab (Soliris®)
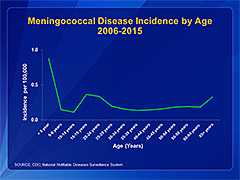
Anyone can get meningococcal disease, but rates of disease are highest in children younger than 1 year old, followed by a second peak in adolescence (see graph below). Among adolescents and young adults, those 16 through 23 years old have the highest rates of meningococcal disease.
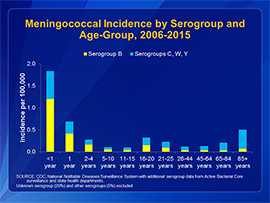
The proportion of cases caused by each serogroup varies by age group. Serogroup B causes approximately 60% of cases among children less than 5 years old. Serogroups C, Y, or W, which are covered by meningococcal conjugate vaccines, cause approximately two out of three cases of meningococcal disease among persons 11 years old and older.
Surveillance Systems
Meningococcal disease is a reportable condition in all states, with cases immediately reported to the local and state health departments. CDC closely tracks meningococcal disease through the National Notifiable Diseases Surveillance System and Active Bacterial Core surveillance.
In 2015, CDC implemented enhanced meningococcal surveillance. The goals for enhanced meningococcal disease surveillance are to:
- Collect more complete data on key variables for monitoring meningococcal disease epidemiology
- Inform vaccine policy decisions
- Collect meningococcal isolates from a broad and representative population
Data and isolates are now routinely collected from most state and large jurisdiction health departments.
The most recent Council of State and Territorial Epidemiologists (CSTE) case classification (2015) for meningococcal disease is:
Suspected
- Clinical purpura fulminans in the absence of a positive blood culture; or
- Gram-negative diplococci, not yet identified, isolated from a normally sterile body site (e.g., blood or cerebrospinal fluid [CSF])
Probable
- Detection of Neisseria meningitidis antigen
- In formulin-fixed tissue by immunohistochemistry (IHC); or
- In CSF by latex agglutination
Confirmed
- Detection of N. meningitidis-specific nucleic acid in a specimen obtained from a normally sterile body site (e.g., blood or CSF), using a validated polymerase chain reaction (PCR) assay; or
- Isolation of N. meningitidis
- From a normally sterile body site (e.g., blood or CSF, or less commonly, synovial, pleural, or pericardial fluid); or
- From purpuric lesions.
Enhanced Meningococcal Disease Surveillance Reports
View meningococcal disease data, including case counts and incidence by serogroup and age, vaccination history of cases, meningococcal related deaths, incidence by serogroup and college attendance, and HIV status.
Related Pages
-
- Surveillance Manual’s Chapter on Meningococcal Disease
-
Active Bacterial Core surveillance Reports
(see Neisseria meningitidis)
- Page last reviewed: March 28, 2017
- Page last updated: September 15, 2017
- Content source:
- Content source: National Center for Immunization and Respiratory Diseases


 ShareCompartir
ShareCompartir