Pathogens and Diseases
Data and Reports
- How human antibiotic resistance has changed over the last two decades
- Estimated annual number of illnesses caused by 31 pathogens (from 2011 estimates report) [PDF – 1 page]
- Estimated annual number of hospitalizations and deaths caused by 31 pathogens (from 2011 estimates report) [PDF – 1 page]
- CDC’s report on antibiotic resistance threats in the United States
CDC, through NARMS, monitors antibiotic resistance in several types of bacteria that are transmitted commonly through food. This page describes these pathogens and the importance of monitoring their resistance to antibiotics.
Estimates of incidence, hospitalizations, and deaths are from the 2011 CDC Estimates of Foodborne Illness in the United States.
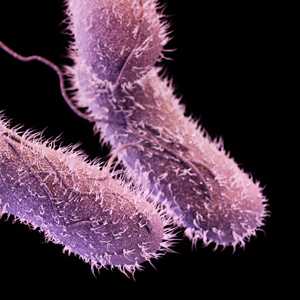
Salmonella, non-typhoidal serotypes
Most people infected with non-typhoidal Salmonella bacteria develop diarrhea, fever, and abdominal cramps. An estimated 1.2 million people get sick from Salmonella infection in the United States each year. Of these, about 23,000 are hospitalized, and 450 die from their infections.
Many of these infections are foodborne.
- Young children, older adults, and persons with weakened immune systems are most likely to have severe illness.
- Infections usually do not require any treatment other than oral fluids, but antibiotics are used when the bacteria have spread from the intestines, e.g., to the blood.
- Increasing resistance to clinically important antibiotics, such as cephalosporins, presents a challenge for treatment.
The risk of getting a Salmonella infection can be decreased by thoroughly cooking food, especially foods of animal origin (i.e., beef, poultry, milk, eggs), and washing hands and surfaces during meal preparation and after contact with animals or their environments.
Salmonella serotype Typhi (the agent of Typhoid Fever)
Typhoid fever is a life-threatening illness caused by Salmonella serotype Typhi bacteria. Symptoms include a sustained fever as high as 104°F, weakness, stomach pains, headache, and loss of appetite.
Typhoid fever is still common in many developing countries, where it affects about 21.5 million persons each year. In the United States, an estimated 5,700 cases occur each year, and about 75% of these are acquired while traveling internationally.
Resistance to one or more antibiotics tested in NARMS has increased in the last 10 years. Most of this increase is due to rising resistance to quinolone antibiotics like ciprofloxacin, which are commonly used for treatment of typhoid fever.
The chance of getting typhoid fever is very low in the United States. When traveling in a country where typhoid fever is common, risk of infection can be decreased through vaccination, eating only food that is cooked and served hot, choosing fruits and vegetables that you have washed in clean water or peeled yourself, and drinking only beverages made with boiled or disinfected tap water.
Campylobacter
Most people who become ill from Campylobacter get diarrhea, cramping, abdominal pain, and fever two to five days after ingesting the bacteria. The diarrhea may be bloody and can be accompanied by nausea and vomiting. Rarely, Campylobacter infection results in longer-term consequences, such as arthritis or a type of paralysis called Guillain-Barré syndrome that can last for weeks or months.
Campylobacter is estimated to cause over 1.3 million illnesses and 76 deaths in the United States each year.
- Young children, older adults, and persons with weakened immune systems are most likely to have severe illness.
- An increasing percentage of Campylobacter bacteria infecting humans are resistant to quinolones, a class of drugs that is important for treating severe infections.
The risk of getting a Campylobacter infection can be decreased by cooking poultry thoroughly, preventing cross-contamination from poultry to other foods, not drinking raw milk, and drinking only water that has been treated.
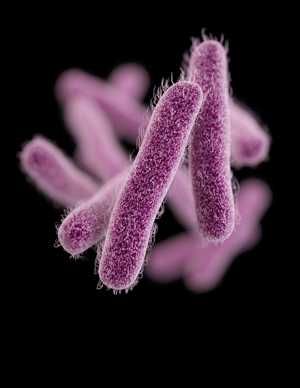
Shigella
Most people who are infected with Shigella develop diarrhea, fever, and stomach cramps starting a day or two after they are exposed to the bacteria. The diarrhea is often bloody. Some infected persons have no symptoms at all, but may still pass the bacteria to others.
About 14,000 cases of Shigella infection are reported each year in the United States, but the actual number of illnesses is estimated to be about 20 times greater, because mild cases are often not diagnosed or reported.
These bacteria are not carried by animals.
- Transmission typically occurs when one person’s invisible fecal matter contaminates a surface; others touch it, and then put fingers in their mouths.
- This is most common in child-care settings where children are not toilet-trained.
- Recovery is common without antibiotics, but antibiotics can be lifesaving to someone with severe illness or a weakened immune system.
- Many Shigella infections in children are resistant to at least one of the antibiotics approved for treatment.
There is no vaccine to prevent shigellosis, but the chance of getting the infection can be decreased by washing hands carefully and frequently.
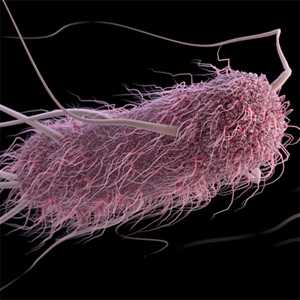
Escherichia coli (E. coli)
E. coli bacteria normally live in the intestines of people and animals. Most E. coli strainsare harmless and are actually an important part of a healthy human intestinal tract. However, some E. coli are pathogenic, meaning they can cause diarrhea or illness in parts of the body outside the intestinal tract.
Shiga toxin-producing E. coli (STEC), which includes E. coli O157, can cause severe disease. An estimated 265,000 STEC infections and 3600 hospitalizations occur each year in the United States.
Antibiotics are not recommended for treating STEC infections, but resistant E. coli have the potential to transfer their resistance to other types of bacteria. In 2011, about 3 of every 100 human E. coli O157 isolates were resistant to at least 5 classes of antibiotics.
The chance of getting an E. coli infection can be decreased by:
- Cooking beef, especially ground beef thoroughly
- Washing hands frequently, especially after contact with young ruminant animals
- Not drinking raw milk
- Drinking only water that has been disinfected.
Vibrio species
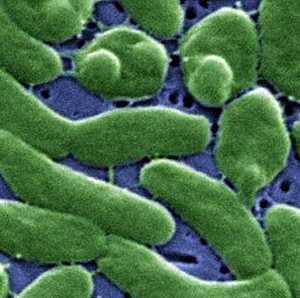
Vibrio parahaemolyticus and Vibrio vulnificus are two species of bacteria in the same family as the bacteria that cause cholera. They live in saltwater environments.
Vibrio parahaemolyticus typically causes watery diarrhea, abdominal cramping, nausea, vomiting, fever, and chills. An estimated 45,000 cases of V. parahaemolyticus infection occur annually in the United States.
- V. vulnificus is less common but frequently causes life-threatening infections, including severe wound infections and bloodstream infections.
- Persons with liver disease or weakened immune systems are at higher risk for V. vulnificus infection.
People usually get infected (with either Vibrio) by eating contaminated seafood, particularly raw oysters, or (for Vibrio vulnificus) by exposing an open wound to seawater that contains the bacteria. Antibiotics are needed for some persons with V. parahaemolyticus infection and for anyone with V. vulnificus infection.
The risk of getting these infections can be decreased by:
- Not eating raw shellfish
- Making sure that cooked foods do not get cross-contaminated by raw shellfish
- Avoiding exposure of open wounds to saltwater or brackish water (for persons with liver disease or compromised immune systems).
- Page last reviewed: August 19, 2015
- Page last updated: August 19, 2015
- Content source:


 ShareCompartir
ShareCompartir