Antibiotic Resistance Threats Report and Foodborne Germs

This web page provides a brief overview of how CDC’s Antibiotic Resistance Threats in the United States, 2013 report [PDF – 114 pages, 5.24 MB] connects antibiotic resistance to foodborne and other enteric germs in animals, food, and humans.
In the report, CDC calls for four core actions to fight antibiotic resistance:
- Preventing Infections, Preventing the Spread of Resistance
- Tracking Resistance Patterns
- Improving Use of Today’s Antibiotics (Antibiotic Stewardship)
- Developing New Antibiotics and Diagnostic Tests
The report includes 2-page fact sheets on 18 drug-resistant threats that are ranked in categories of urgent, serious, and concerning. The urgent threats are CRE, C. difficile, and drug-resistant gonorrhea.
Foodborne infections cited in the report are drug-resistant Campylobacter [PDF – 114 pages, 5.24 MB], non-typhoidal Salmonella [PDF – 114 pages, 5.24 MB], Salmonella Typhi [PDF – 114 pages], and Shigella [PDF – 114 pages] and are ranked under the serious category.
Preventing Infections: CDC’s Work to Prevent Antibiotic Resistance in Food
Each year, millions of people in the United States become sick from foodborne and other enteric (gastrointestinal) infections. While many of these infections are mild and do not require treatment, antibiotics can be lifesaving in severe infections. Antibiotic resistance compromises our ability to treat these infections and is a serious threat to public health.1
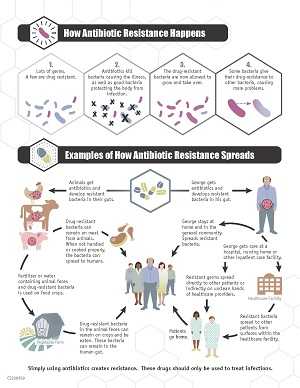
- The germs that contaminate food can be resistant because of the use of antibiotics in people and in food animals.
- For some germs, like the bacteria Salmonella and Campylobacter, it is primarily the use of antibiotics in food animals that increases resistance.
- We can prevent many of these resistant infections with careful antibiotic use and by keeping Salmonella and other bacteria out of the food we eat.
- Recent outbreaks in 2011, 2011-2012, and 2013 of multi-resistant Salmonella traced to ground beef and poultry show how animal and human health are linked.
Resistant Genes and Antibiotics
There is concern that use of antibiotics in any setting can select for resistance in other bacteria that do not themselves cause disease, but that can share those resistance genes with bacteria that do.
The origin of resistant genes is often not known, but they can sometimes naturally be in germs in soil. The selection process that makes them more common happens in settings where antibiotics are used a lot: hospitals, the community, and food animal production.
“Resistant bacteria in food-producing animals are of particular concern because these animals serve as carriers.” Threats report
Antibiotic Use in Agriculture
Antibiotics are widely used in food-producing animals. The 2013 Threats report points out that according to data published by FDA, there are more kilograms of antibiotics sold in the United States for food-producing animals than for people.1,2 This use contributes to the emergence of antibiotic-resistant bacteria in food-producing animals.1
Genes don’t stay put
Scientists around the world have provided strong evidence that antibiotic use in food-producing animals can harm public health.1 Resistant bacteria can contaminate the foods that come from animals that serve as carriers of resistant bacteria, and people who consume these foods can develop antibiotic-resistant infections.1
“There are commonalities in how to counter things in terms of prevention and outbreak control, detection and stewardship, but there are important differences.” says Dr. Thomas Frieden.
It is important to have a better understanding of the flow of resistant genes—from the hospital ward to our communities, from one country to another, and from farms to people.
We are beginning to track the movement of the genes themselves using molecular methods. For example, the same exact gene in Salmonella from food animals has been found in meat and poultry bought in grocery stores and in sick people.3
Why is this important?
“Scientists around the world have provided strong evidence that antibiotic use in food-producing animals can have a negative impact on public health.”
Because of the link between antibiotic use in food-producing animals and the occurrence of antibiotic-resistant infections in humans, antibiotics that are medically important to treating infections in humans should be used in food-producing animals only under veterinary oversight and only to manage and treat infectious diseases, not to promote growth.1
What can we do?
Antibiotics must be used judiciously in humans and animals because both uses contribute to not only the emergence, but also the persistence and spread of antibiotic-resistant bacteria.1
Preventing the spread of antibiotic resistance can only be achieved with widespread engagement, especially among leaders in clinical medicine, healthcare leadership, agriculture, and public health.1
More Information:
Key CDC resources highlighting the Threats report:
- CDC’s Work to Prevent Antibiotic Resistance in Food [PDF – 114 pages, 5.24 MB]
- Erratum in: Antibiotic Resistance Threats in the United States, 2013: Technical Appendix [PDF – 114 pages, 5.24 MB]
- References 2 and 3 for drug resistant non-typhoidal Salmonella should be switched on p. 99.
- CDC feature
- Press Release
- Digital Press Kit
- Pinterest page with illustrations and graphics
Foodborne (and enteric) pathogen pages:
In the media
- CDC Threat Report: Yes, Agricultural Antibiotics Play a Role in Drug Resistance
- Antibiotic-Resistant ‘Superbugs’ Pose Urgent Threat to Public Health: CDC
- CDC Report on Antibiotic Resistance in the U.S. Should Be a “Wake-Up Call” on Factory Farms
- Study: Livestock drugs, hardier bugs
- Will the Medicine Cabinet Be Empty When You or Your Child Need Life-Saving Antibiotics? (Slideshow)
- CDC report shows growing threat posed by antibiotic resistance
- It’s Official – Again: CDC report on antibiotic resistance warns of “potentially catastrophic consequences of inaction”
- Where superbugs come from: CDC report reiterates that misuse of antibiotics in agriculture plays a role
- Emerging Pathogens: Antibiotic Resistance Slowly Growing in Salmonella
- Taking antibiotics you don’t really need might kill you
- Antibiotic-Resistant Infections Lead to 23,000 Deaths a Year, C.D.C. Finds
References
- CDC. Antibiotic Resistance Threats in the United States, 2013. Atlanta, GA; 2013. p. 7, 36-7
- Center for Veterinary Medicine at FDA. 2011 Summary Report on Antimicrobials Sold or Distributed for Use in Food-Producing Animals [PDF – 4 pages] .
- Sjolund-Karlsson M, Howie RL, Blickenstaff K, Boerlin P, Ball T, Chalmers G, Duval B, Haro J, Rickert R, Zhao S, Fedorka-Cray PJ, Whichard JM. Occurrence of beta-lactamase genes among non-Typhi Salmonella enterica isolated from humans, food animals, and retail meats in the United States and Canada. Microbial drug resistance. Microbial drug resistance. 2013;19(3):191-7.
- Page last reviewed: October 21, 2013
- Page last updated: April 14, 2014
- Content source:


 ShareCompartir
ShareCompartir