Data & Statistics for Cerebral Palsy
Prevalence and Characteristics
- Cerebral palsy (CP) is the most common motor disability in childhood. 1
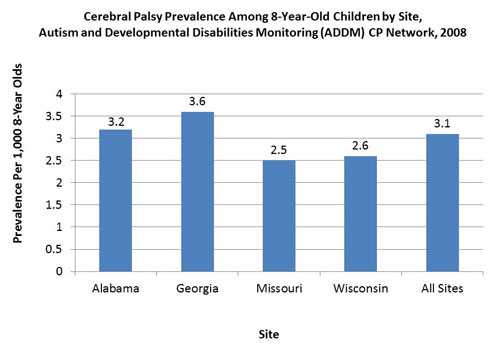
- Population-based studies from around the world report prevalence estimates of CP ranging from 1.5 to more than 4 per 1,000 live births or children of a defined age range. (2, 3, 4, 5,6)
- About 1 in 323 children has been identified with CP according to estimates from CDC’s Autism and Developmental Disabilities Monitoring (ADDM) Network. [Read summary]
 [D]
[D]
- CDC tracks CP through the Autism and Developmental Disabilities Monitoring (ADDM) CP Network.
- In 2008, the ADDM CP Network included areas of Alabama, Georgia, Missouri, and Wisconsin. Based on children who were 8 years old and living in these four communities in 2008, the ADDM CP data showed that: [Read summary] [ Read Community Report]
- CP was more common among boys than among girls.
- CP was more common among Black children than White children. Hispanic and White children were about equally likely to have CP.
- Most (77.4%) of the children identified with CP had spastic CP.
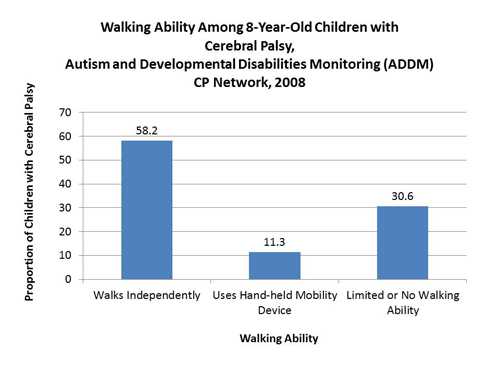
- Over half (58.2%) of the children identified with CP could walk independently.
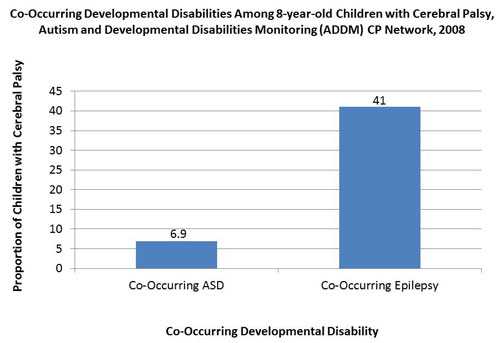
- Many of the children with CP also had at least one co-occurring condition—41% had co-occurring epilepsy and 6.9% had co-occurring ASD.
Walking Ability
- In 2008, 58.2% of children with CP could walk independently, 11.3% walked using a hand-held mobility device, and 30.6% had limited or no walking ability. [Read summary]
 [D]
[D]
- According to 2006 data from the ADDM CP Network, Black children with cerebral palsy were 1.7 times more likely to have limited or no walking ability compared with White children. [Read summary]
- Another study found that 41% of children with CP were limited in their ability to crawl, walk, run, or play, and 31% needed to use special equipment such as walkers or wheelchairs. [Read article]
Co-Occurring Developmental Disabilities
- Almost half (41%) of the children identified with CP by the ADDM CP Network had co-occurring epilepsy. Co-occurring epilepsy frequency was highest among children with cerebral palsy who had limited or no waking ability. [Read summary]
- Some (6.9%) of the children identified with CP also had autism spectrum disorder (ASD). Co-occurring ASD frequency was higher among children with non-spastic CP, particularly hypotonic CP. [Read summary]
- It is important to note that the overall identified prevalence of ASD among children in the US is about 1% (7). That means that the identified prevalence of ASD among children with CP is much higher than among their peers without CP.
 [D]
[D]
- The ADDM site that tracks CP in metropolitan Atlanta is the Metropolitan Atlanta Developmental Disabilities Surveillance Program (MADDSP). MADDSP 2006 data show that:
- Approximately 60% of 8-year-old children with CP had another developmental disability.
- More than 40% of children with CP had intellectual disability, 35% had epilepsy, and more than 15% had vision impairment. Nearly 1 in 4 children with CP had both intellectual disability and epilepsy.
Risk Factors
Low Birthweight and Premature Birth
- A study in metropolitan Atlanta found that the prevalence of CP was 6.2 per 1,000 livebirths among children born weighing 1,500 to 2,499 grams (3⅓ to 5½ pounds) and 59.5 per 1,000 livebirths among children born weighing less than 1,500 grams, compared with 1.1 per 1,000 for children born weighing 2,500 grams or more. [Read article]
- In data from Europe and Australia, the prevalence of CP ranged from: (8)
- 35.0 to 79.5 per 1,000 live births for children born at 28 to 31 weeks gestation
- 1.1 to 1.7 per 1,000 live births for children born at 37 or more weeks gestation
- In data from Sweden, the prevalence of CP was: (8)
- 43.7 per 1,000 live births for children born at 28 to 31 weeks gestation
- 6.1 per 1,000 live births among children born at 32 to 36 weeks gestation
- 1.4 per 1,000 live births for children born at 37 or more weeks gestation
- A study in Scotland found that children born as part of a multiple birth pregnancy such as being a twin were found to be almost five times more likely to have CP than children born as singletons. Part, but not all, of this increased risk is due to the fact that multiple birth children are more likely to be born prematurely or at low birthweight. [Read summary]
- A study in Denmark found that children born after in vitro fertilization (assisted conception) were 1.6 times as likely to have CP, due to the fact that they were more likely to be born prematurely or from a multiple pregnancy. [Read article]
Disruption of Blood and Oxygen Supply to the Developing Brain
- Ischemic stroke, when a blood clot blocks a blood vessel in the brain, is recognized to cause brain damage that can result in CP. It can occur in the developing fetal brain during pregnancy or shortly after birth. [Read summary]
- Disruption of the oxygen supply during birth (birth hypoxia) has been estimated to account for less than 10% of CP cases. [Read summary]
Infection Among Mothers
- Infection of the placental membranes (chorioamnionitis) or other signs of infection (blood infection in the mother or fever during labor) have been associated with an increased risk of CP for children born full-term. [Read article], [Read summary]
- Chorioamnionitis has been found to account for 12% of spastic CP among children born full-term and 28% of CP among children born prematurely. [Read article]
- Maternal genitourinary infection has been associated with an increased risk of CP among children born prematurely or at low birthweight. [Read article]
Other Factors
- Birth defects of the central nervous system (brain) were found to be more common among children with CP than among those without CP. [Read summary]
- Data from metropolitan Atlanta showed that about 10% to 15% of CP was acquired in the early years of a child’s life. The most frequent causes were brain injuries from motor vehicle crashes or falls, and infections (such as meningitis). [Read article], [Read summary]
Economic Costs
- Among children enrolled in Medicaid in 2005, medical costs were higher for children with cerebral palsy. Costs were highest for children with both cerebral palsy and intellectual disability. [Read summary]
- Medical costs for children with cerebral palsy alone were 10 times higher than for children without cerebral palsy or intellectual disability ($16,721 vs. $1,674 in 2005 dollars).
- Medical costs for children with both cerebral palsy and intellectual disability were 26 times higher than for children without cerebral palsy or intellectual disability ($43,338 vs. $1,674 in 2005 dollars).
- CDC has estimated that the lifetime cost to care for an individual with CP is nearly $1 million (2003 dollars). [Read article]
- It also has been estimated that the combined lifetime costs for all people with CP who were born in 2000 will total $11.5 billion in direct and indirect costs. [Read article]
Highlighted Articles
Key Findings: Birth Prevalence of Cerebral Palsy
The journal, Pediatrics, has published a CDC study that looked over time at how often cerebral palsy (CP) occurred in the population, also known as the birth prevalence of CP.
(Published: December 9, 2015)
Key Findings: Prevalence of cerebral palsy, co-occurring autism spectrum disorders, and motor functioning
The Developmental Medicine and Child Neurology journal has published a new study: “Prevalence of Cerebral Palsy, Co-Occurring Autism Spectrum Disorders, and Motor Functioning – Autism and Developmental Disabilities Monitoring Network, USA, 2008.”
(Published: October 22, 2013)
11 Things to Know About Cerebral Palsy
Learn more about CP and what signs to look for in young children.
(Published: March 13, 2017)
Living with Cerebral Palsy: The Gandee Family Story
Read one family’s experience living with CP.
(Published March 23, 2016)
Cerebral Palsy Quiz
How much do you know about cerebral palsy? Take a quiz to find out and read one family’s personal experience with the condition.
(Published: March 3, 2015)
Dalila’s Story
Read one woman’s story about how her cerebral palsy gives her strength.
(Published: January 16, 2015)
What you Need to Know About Cerebral Palsy
Learn more about this condition and what professionals who serve young children can do.
(Published: March 3, 2014)
Are you prepared?
One family’s story how emergency preparedness can affect children with special health care needs.
(Published: September 23, 2013)
Cerebral Palsy: One Parent’s Story
Read about one family’s experience with cerebral palsy.
(Published: March 19, 2012)
References
- Capute and Accardo’s Neurodevelopmental Disabilities in Infancy and Childhood, Third Edition. Edited by Pasquale J. Accardo, MD. 2008, Paul H. Brookes Publishing Co, Baltimore, MD. p17.
- Arneson CL, Durkin MS, Benedict RE, Kirby RS, Yeargin-Allsopp M, Van Naarden Braun K, Doernberg NS. (2009). Prevalence of Cerebral Palsy: Autism and Developmental Disabilities Monitoring Network, Three Sites, United States, 2004. Disability and Health Journal, 2(1), 45–48.
- Bhasin TK, Brocksen S, Avchen RN, Van Naarden Braun K. (2006). Prevalence of four developmental disabilities among children aged 8 years – Metropolitan Atlanta Developmental Disabilities Surveillance Program, 1996 and 2000. MMWR. Surveillance Summaries, 55(1), 1–9.
- Paneth N, Hong T, Korzeniewski S. (2006). The descriptive epidemiology of cerebral palsy. Clinics in Perinatology, 33(2), 251–267.
- Surveillance of Cerebral Palsy in Europe. (2002). Prevalence and characteristics of children with cerebral palsy in Europe. Developmental Medicine and Child Neurology, 44(9), 633–640.
- Winter S, Autry A, Boyle C, Yeargin-Allsopp M. (2002). Trends in the prevalence of cerebral palsy in a population-based study. Pediatrics, 110(6), 1220–1225.
- CDC. (2012). Prevalence of autism spectrum disorders—Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveillance Summaries, 61(3), 1-19.
- Pakula AT, Van Naarden Braun K, Yeargin-Allsopp M. “Cerebral plasy: classification and epidemiology,” in Cerebral Palsy, Volume 20, Number 3. Edited by Linda J. Michaud, MD, PT. 2009, W.B. Saunders Company, Philadelphia, PA. p437.
- Page last reviewed: February 3, 2017
- Page last updated: May 2, 2016
- Content source:


 ShareCompartir
ShareCompartir