Asia Field Program
The Centers for Disease Control and Prevention (CDC) has collaborated with the Thailand Ministry of Public Health (MoPH) for over 30 years. This collaboration has led to new prevention and control strategies that have had significant global public health impacts, especially in the areas of HIV, influenza, tuberculosis, and emerging infectious diseases.
As the newest member of this collaboration, the Immigrant, Refugee, and Migrant Health (IRMH) Branch, part of CDC’s Division of Global Migration and Quarantine (DGMQ), conducts surveillance activities, responds to disease outbreaks, strengthens international partnerships, and conducts local outreach and health education activities through its Asia Field Program. Two of its primary activities center on the Mae Sot Processing Center and the Mae La refugee camp, both located in Western Thailand bordering Burma.
Mae Sot Processing Center for U.S.-Bound Refugees

Mae Sot Processing Center and Mae La Refugee Camp, both located near the Thailand-Burma border.
Since 2004, more than 60,000 refugees from Burma have resettled from Thailand to the United States. For all such refugees coming to the United States, a medical examination is mandatory to identify, for the Department of State and the U.S. Citizenship and Immigration Service, applicants with inadmissible conditions. These include communicable diseases of public health concern (notably TB disease, which requires successful completion of treatment prior to resettlement), physical and mental disorders with associated harmful behaviors, and substance abuse and addiction.
CDC’s Division of Global Migration and Quarantine (DGMQ) develops and implements the medical screening guidelines, called Technical Instructions, used to conduct the exams. For refugees living in five refugee camps along the Thai-Myanmar border (including Mae La), these exams are conducted by physicians from the International Organization for Migration (IOM) at the Mae Sot Processing Center about 3-6 months before departure. With guidance from DGMQ, IOM also conducts pre-departure screenings 1-3 weeks before departure and pre-embarkation checks (fit-to-fly checks) 1-3 days before departure.
DGMQ Public Health Activities
Managing Infectious Threats: DGMQ provides on-going guidance to IOM on how to manage infectious threats to the U.S.-bound population during processing at the center. In an outbreak setting, such instructions can encompass treatment, prophylaxis, isolation, and/or travel restrictions.
Vaccination and Presumptive Treatment: DGMQ developed evidence-based recommendations for pre-departure vaccinations, which are not mandatory for resettlement, and presumptive treatment with albendazole and ivermectin. At least one-third of the world’s population is infected with intestinal parasites, making it one of the most common conditions detected in refugees newly arriving to the United States. A successful pilot program to provide presumptive treatment for strongyloides infection with ivermectin for refugees originating from Asia helped DGMQ reach a cost-sharing agreement with the Department of State Bureau of Population, Refugees, and Migration. The International Organization of Migration will be funded to provide presumptive treatment for every refugee population at high risk for strongyloides. DGMQ will lead efforts to expand ivermectin presumptive treatment for all U.S.-bound refugees.
DGMQ’s science and expertise in disease detection was a successful precursor in changing the overseas public health screening and treatment of parasitic infections for refugees. Presumptive treatment represents a cost-effective and low burden method of protecting and improving refugee health.
Enhanced Medical Exam: DGMQ, in collaboration with IOM, is currently piloting and evaluating a voluntary testing and treatment program for certain medical conditions during the mandatory exam. These conditions include intestinal parasites, anemia, and chronic hepatitis B virus infection. Positive results do not affect resettlement because these are not inadmissible conditions. Rather, testing would benefit the refugee, which will in turn benefit the receiving community.
Mae La Refugee Camp
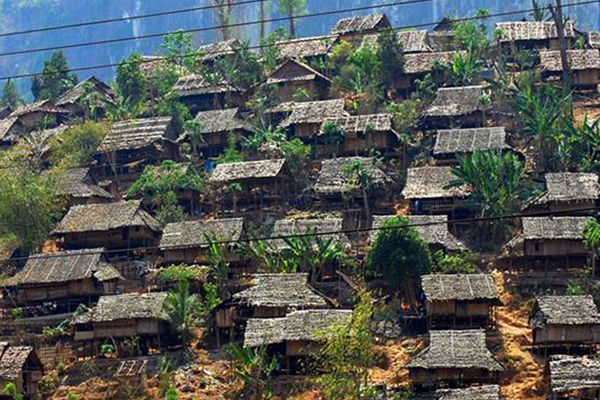
Mae La Refugee Camp, home to 45,000 Karen refugees.
Established in 1984, Mae La Refugee Camp is one of nine refugee camps along the Thai-Myanmar border. The camp has the largest refugee population, close to 45,000 Karen refugees in a four-square-kilometer area. The camp is administered by the Royal Thai Government while non-governmental organizations (NGOs) provide healthcare, water and sanitation, and other services. Première Urgence–Aide Médicale Internationale, the main healthcare NGO and an important partner for DGMQ, provides care, free-of-charge in a field hospital with a 158-bed inpatient unit and two outpatient clinics.
DGMQ Public Health Activities
Vaccination for Cholera Prevention: Mae La has experienced cholera outbreaks in four of the last eight years. To supplement ongoing water and sanitation improvements with immunization using a new and more affordable oral cholera vaccine, DGMQ forged a coalition among Thai Ministry of Public Health (MOPH), Première Urgence – Aide Médicale, and Bill and Melinda Gates Foundation to deliver and evaluate a campaign for all 45,000 refugees living in Mae La. This project will generate a “road map” for vaccine intervention in similar settings and contribute to the evidence base that will define the public health role of oral cholera vaccination.
Investigation and Recommended Remediation for Lead Poisoning: When U.S. providers reported elevated blood lead levels in refugee children arriving from Thailand, DGMQ conducted a field investigation to identify the cause. Risk factors for elevated blood lead levels included hemoglobin <10 g/dL, exposure to car batteries, and taking traditional medicines. Healthcare NGOs conducted remediation accordingly, and the study prompted a wider investigation by Thai health authorities beyond the camp’s borders.
Strengthening Surveillance and Outbreak Response: DGMQ, in collaboration with the World Health Organizaion and Thai MOPH, provides ongoing technical and training support for healthcare NGOs, leading to stronger public health systems and better coordination between the NGOs and Thai health authorities.
- Page last reviewed: December 23, 2016
- Page last updated: December 23, 2016
- Content source:


 ShareCompartir
ShareCompartir