Diagnosis and Treatment
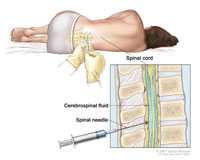
Doctors use a lumbar puncture to collect a sample of cerebrospinal fluid. Larger image.
Doctors consider some pneumococcal infections “invasive.” Invasive disease means that germs invade parts of the body that are normally free from germs.
Early diagnosis and treatment are very important for invasive pneumococcal disease. It is important to know if it is pneumococcal disease because the treatment will change depending on the cause. In the case of pneumococcal disease, antibiotics can help prevent severe illness.
Diagnosis
If doctors suspect invasive pneumococcal disease, like meningitis or bloodstream infections, they collect samples of cerebrospinal fluid or blood and send them to a laboratory for testing.
Identifying pneumococcus bacteria from the sample collected helps doctors confirm that pneumococcus is the cause of the illness. Additionally, growing the bacteria in a laboratory is important for identifying the specific type of bacteria that is causing the infection. It’s also important for deciding which antibiotic will work best.
For non-invasive pneumococcal pneumonia in adults, there is also a urine test that can help to make the diagnosis. For other pneumococcal infections, like ear and sinus infections, healthcare professionals usually diagnose them based on a history and physical exam findings that support pneumococcal infection.
Treatment
Antibiotics can treat pneumococcal disease. However, many types of pneumococcal bacteria have become resistant to some of the antibiotics used to treat these infections. Available data [5.24 MB, 114 pages] show that pneumococcal bacteria are resistant to one or more antibiotics in 3 out of every 10 cases.

Pneumococcal bacteria are resistant to one or more antibiotics in 3 out of every 10 cases.
Antibiotic sensitivity testing shows which antibiotics will be most successful at treating a bacterial infection.
Antibiotic treatment for invasive pneumococcal infections typically includes ‘broad-spectrum’ antibiotics until results of antibiotic sensitivity testing are available. Broad-spectrum antibiotics work against a wide range of bacteria. Once the sensitivity of the bacteria is known, a more targeted (or ‘narrow spectrum’) antibiotic may be selected.
With success of the pneumococcal conjugate vaccine, we see much less antibiotic-resistant pneumococcal infections. In addition to the vaccine, appropriate use of antibiotics may also slow or reverse drug-resistant pneumococcal infections.
- Page last reviewed: September 6, 2017
- Page last updated: September 6, 2017
- Content source:


 ShareCompartir
ShareCompartir