Information for Clinicians
Presentation
Relapsing Fever Bacteria
Relapsing fever is caused by certain species of Borrelia, a gram negative bacteria 0.2 to 0.5 microns in width and 5 to 20 microns in length. They are visible with light microscopy and have the cork-screw shape typical of all spirochetes. Relapsing fever spirochetes have a unique process of DNA rearrangement that allows them to periodically change the molecules on their outer surface. This process, called antigenic variation, allows the spirochete to evade the host immune system and cause relapsing episodes of fever and other symptoms. Three species cause TBRF in the United States: Borrelia hermsii, B. parkerii, and B. turicatae. The most common cause is cause is B. hermsii.
Tick-borne relapsing fever is characterized by recurring febrile episodes that last ~3 days and are separated by afebrile periods of ~7 days duration. Along with fever, patients may experience a wide range of nonspecific symptoms (Table 1). Each febrile episode ends with a sequence of symptoms collectively known as a “crisis.” During the “chill phase” of the crisis, patients develop very high fever (up to 106.7°F or 41.5°C) and may become delirious, agitated, tachycardic and tachypneic. Duration is 10 to 30 minutes. This phase is followed by the “flush phase”, characterized by drenching sweats and a rapid decrease in body temperature. During the flush phase, patients may become transiently hypotensive. Overall, patients who are not treated will experience several episodes of fever before illness resolves.
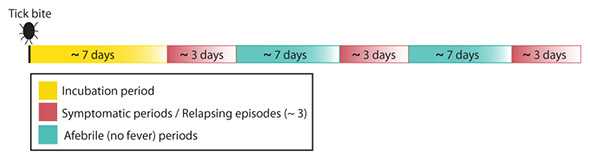
General timeline for TBRF relapse intervals.
Physical Exam
Findings on physical exam vary depending on the severity of illness and when the patient seeks medical care. Regardless, there are no findings specific for TBRF. Patients typically appear moderately ill and may be dehydrated. Occasionally a macular rash or scattered petechiae may be present on the trunk and extremities. Less frequently, patients may have jaundice, hepatosplenomegaly, meningismus, and photophobia (Table 1). Although less common, infection with B. turicatae is especially likely to result in neurologic involvement.
Table 1. Selected Symptoms and Signs among Patients with Tick-borne Relapsing Fever, United States*
| Symptom | Frequency of Symptom | Sign | Frequency of Sign |
|---|---|---|---|
| Headache | 94% | Confusion | 38% |
| Myalgia | 92% | Rash | 18% |
| Chills | 88% | Jaundice | 10% |
| Nausea | 76% | Hepatomegaly | 10% |
| Arthralgia | 73% | Splenomegaly | 6% |
| Vomiting | 71% | Conjunctival Injection | 5% |
| Abdominal pain | 44% | Eschar | 2% |
| Dry cough | 27% | Meningitis | 2% |
| Eye pain | 26% | Nuchal rigidity | 2% |
| Diarrhea | 25% | ||
| Photophobia | 25% | ||
| Neck pain | 24% |
*Abstracted from Dworkin, M. S., et al. Tick-borne relapsing fever in the northwestern United States and southwestern Canada. Clinical Infectious Diseases 1998; 26: 122-31.
Laboratory Testing
Spirochetemia (spirochetes in blood) in TBRF often reaches high concentrations, 100-1000 times more than in cases of early Lyme disease. Thus, microscopy is a useful diagnostic tool for TBRF. The definitive diagnosis of TBRF may be based on the observation of relapsing fever spirochetes (Borrelia hermsii, B. turicatae, or B. parkerii in the US) in peripheral blood smears of a symptomatic person by a microscopist trained in spirochete identification. Although best visualized by dark field microscopy, the organisms can also be detected using Wright-Giemsa or acridine orange stains.
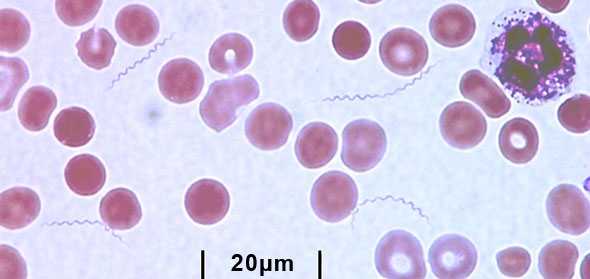
Peripheral blood smear. The TBRF bacteria are long and spiral-shaped. The circular objects are red blood cells. The irregular purple object in the top right corner is a white blood cell.
The organisms are best detected in blood obtained while a person is febrile. With subsequent febrile episodes, the number of circulating spirochetes decreases, making it harder to detect spirochetes on a peripheral blood smear. Even during the initial episode spirochetes will only be seen 70% of the time.
Blood samples obtained before antibiotic treatment can be cultured using BSK (Barbour Stoner Kelly) medium or by inoculating immature mice. The spirochete will usually be evident within 24 hours if the blood was drawn during a febrile episode.
Although not valuable for making an immediate diagnosis, serologic testing is available through public health laboratories and some private laboratories. Acute serum should be taken within 7 days of symptom onset and convalescent serum should be taken at least 21 days after symptoms start. Early antibiotic treatment may blunt the antibody response and the antibody levels may wane quickly during the months after exposure. To confirm the diagnosis of TBRF, Borrelia specific antibody titers should increase 4-fold between acute and convalescent serum samples, and convalescent serum antibody levels should be at least two standard deviations above pooled negative controls. Serologic testing for TBRF is not standardized and results may vary by laboratory. Patients with TBRF may have false-positive tests for Lyme disease because of the similarity of proteins between the two organisms.
Incidental laboratory findings include normal to increased white blood cell count with a left shift towards immature cells, a mildly increased serum bilirubin level, mild to moderate thrombocytopenia, elevated erythrocyte sedimentation rate (ESR), and slightly prolonged prothrombin time (PT) and partial thromboplastin time (PTT).
Treatment of Tick-borne Relapsing Fever
TBRF spirochetes are susceptible to penicillin and other beta-lactam antimicrobials, as well as tetracyclines, macrolides, and possibly fluoroquinolones. CDC has not developed specific treatment guidelines for TBRF; however, experts generally recommend tetracycline 500 mg every 6 hours for 10 days as the preferred oral regimen for adults. Erythromycin, 500 mg (or 12.5 mg/kg) every 6 hours for 10 days is an effective alternative when tetracyclines are contraindicated. Parenteral therapy with ceftriaxone 2 grams per day for 10-14 days is preferred for patients with central nervous system involvement, similar to early neurologic Lyme disease. In contrast to TBRF, LBRF caused by B. recurrentis can be treated effectively with a single dose of antibiotics.
When initiating antibiotic therapy, all patients should be observed during the first 4 hours of treatment for a Jarisch-Herxheimer reaction. The reaction, a worsening of symptoms with rigors, hypotension, and high fever, occurs in over 50% of cases and may be difficult to distinguish from a febrile crisis. Cooling blankets and appropriate use of antipyretic agents may be indicated. In addition acute respiratory distress syndrome requiring intubation has been described recently in several patients undergoing treatment for TBRF.
Complications and Prognosis
Given appropriate treatment, most patients recover within a few days. Long-term sequelae of TBRF are rare but include iritis, uveitis, cranial nerve and other neuropathies.
Tick-borne Relapsing Fever in Pregnancy
TBRF contracted during pregnancy can cause spontaneous abortion, premature birth, and neonatal death. The maternal-fetal transmission of Borrelia is believed to occur either transplacentally or while traversing the birth canal. In one study, perinatal infection with TBRF was associated with lower birth weights, younger gestational age, and higher perinatal mortality (Jongen, van Roosmalen et al. 1997).
In general, pregnant women have higher spirochete loads and more severe symptoms than nonpregnant women. Higher spirochete loads have not, however, been found to correlate with fetal outcome.
Immunity
Although there is limited information on the immunity of TBRF, there have been patients who developed the disease more than once.
Public Health Reporting Requirements
Although not a nationally notifiable condition, prompt reporting of TBRF cases is currently required in at least 12 states: Arizona, California, Colorado, Idaho, Montana, North Dakota, Nevada, New Mexico, Oregon, Texas, Utah, and Washington. Regardless of location, health care providers should report cases to appropriate state or local health authorities. Large multistate outbreaks have been linked to rental cabins near national parks and other common vacation locations, and prompt reporting by clinicians was critical to the identification and control of these outbreaks. Without corrective action, tick-infested cabins can remain a source of human infection for many years.
- Page last reviewed: October 15, 2015
- Page last updated: January 8, 2016
- Content source:


 ShareCompartir
ShareCompartir