We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Trochlear nerve palsy
From WikEM
Contents
Background
- Also called the 4th cranial nerve (CN IV)
- Trochlea innervates superior oblique muscle
- Intorts, depresses and abducts the globe
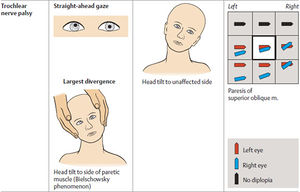
- Trochlear nerve palsy causes an inability to move the eye in inward rotation, downward, and laterally. [1]
- Most common cause of vertical diplopia [2]
Etiology
- Head trauma [3]
- Mechanisms that increase intraocular pressure
- Practically never involved by aneurysm
- Herpes zoster opthalmicus
- Meningitis
- Diabetic neuropathy
- Lupus/Sjogren syndrome
Clinical Features
- Vertical, torsional, or oblique diplopia.
- Worse on downward gaze and gaze away from affected muscle [2]
- Head-tilt
- Ask about history of fever, stiff neck, headache, diabetes, hypertension, other sensory and motor symptoms
Differential Diagnosis
- Increased intracranial pressure (ICP): Pseudotumor cerebri
- Vascular: Stroke, subarachnoid hemorrhage, aneurysm (extremely rare), microvasculopathy signs and symptoms to diabetes, atherosclerosis or hypertension[4]
- Neoplastic: Tumor in the subarachnoid space
- Degenerative/deficiency: Vitamin B deficiency, Wernicke-Korsakoff syndrome
- Idiopathic: Most common cause of acquired trochlear nerve palsy.
- Infection: Meningitis, herpes zoster
- Congenital: Signs/symptoms of dysgenesis of trochlear nerve nucleus or abnormal peripheral nerve
- Autoimmune: Myasthenia gravis, multiple sclerosis, systemic lupus erythematosus, giant cell arteritis, Sjogren’s
- Trauma: Its long course makes it susceptible to traumatic injury. Head trauma (adult) is the second most common cause. Is generally severe with loss of consciousness. Consider underlying structural abnormalities if results after minor trauma.
- Endocrine: Thyroid ophthalmopathy [2] [4]
- Third nerve palsy
- Abducens nerve palsy
Evaluation
Labs and Tests
- +/- POC glucose, CBC, and other labs depending on suspected diagnosis
- +/- LP after negative neuroimaging if suspect subarachnoid hemorrhage or meningitis.
Imaging
- CT Head if traumatic, suspect stroke, or subarachnoid hemorrhage (rare).
- MRI is study of choice, although there no increased yield from MRI vs CT scan. [2] [4]
Management
- Address any acute causes like stroke, trauma
- May require surgical correction
- +/- Neurology consult
Disposition
- Vasculopathic: Observation for improvement over 6-8 weeks. Often resolve spontaneously in 4-6 months.
- Traumatic: Observation for improvement over 6-8 weeks. Often resolves spontaneously. If progressing or lack of improvement – neuroimaging with MRI
- Isolated, idiopathic cases very rarely have an underlying etiology after prolonged follow-up, and most resolve spontaneously in weeks to months. If no improvement in 2 months, consider neuroimaging. [4]
See Also
External Links
Medscape: Trochlear Nerve Palsy
References
- ↑ 1.0 1.1 Marx JA, Hockberger RS, Walls RM, et al., eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. Philadelphia, PA: Mosby/Elsevier; 2013
- ↑ 2.0 2.1 2.2 2.3 Sheik Z. Trochlear Nerve Palsy Treatment and Management on emedicine.medscape.com/article/1200187 Accessed on 8/29/2015
- ↑ Disorders of Ocular Movement and Pupillary Function In: Adams and Victor's Principles of Neurology. 10th ed. Accessed on AccessMedicine.com on 8/29/2015. Chapter 14
- ↑ 4.0 4.1 4.2 4.3 4.4 Brazis, PW. Isolated palsies of cranial nerves III, IV, and VI. Seminars in neurology. 2009 Feb. 29(1):14