Clinical Case Study 1: Fever 6 months after a visit to Pakistan
A 44-year-old man is seen at a physician's office in the United States, during a week-end, for suspected malaria.
The patient was born in Pakistan but has lived in the United States for the past 12 years. He travels frequently back to Pakistan to visit friends and relatives. His last visit there was for two months, returning 11 months before the current episode. He did not take malaria prophylaxis then.
Five weeks ago, he was diagnosed with malaria and treated at a local hospital. The blood smear at that time was reported by the hospital as positive for malaria, species undetermined. He was then treated with 2 days of IV fluids (nature unknown) and tablets (nature unknown), and recovered.
The patient now presents with a history of low grade fever for the past few days, with no other symptoms . A blood smear is taken and examined at a hospital laboratory by the technician (no pathologist is available on this week-end). Through a telephone discussion, the technician states that she sees 4 parasites per 1000 red blood cells, with rings, "other forms with up to four nuclei," and that some of the infected red blood cells are enlarged and deformed.
Question 1: What is your most probable diagnosis?
Not Malaria
That is incorrect. Please, try another answer.
Plasmodium falciparum
That is incorrect. Please, try another answer.
Plasmodium vivax
That is correct.
This is the most probable diagnosis. The reported microscopic findings are compatible with P. vivax: some infected red cells are enlarged and deformed, and the "other forms with four nuclei" are compatible with the presence of schizonts. Plasmodium vivax does occur in Pakistan, where it is found in slightly more than 50% of malaria cases.
The history suggests a relapse of P. vivax malaria, following an earlier episode five weeks ago. The earlier treatment apparently did not include primaquine, thus allowing the persistence of hypnozoites which caused this relapse.
An alternate explanation would be that the earlier infection was caused by chloroquine-resistant P. vivax (which has been reported in Pakistan), with recrudescence of blood-stage parasites occurring after an unsuccessful earlier treatment (if indeed the earlier treatment included chloroquine). However, recrudescences usually occur within 28 days of the intial episode, rather than at five weeks as described here.
The other species are less likely:
- While P. falciparum does occur in Pakistan (slightly less than 50% of malaria cases), this patient reportedly did not develop symptoms until 10 months after departure from the exposure area: most cases of P. falciparum would have become symptomatic earlier.
- P. ovale occurs mainly in Africa and has been found only occasionally in Asia (in the western Pacific).
- P. malariae occurs worldwide, but its distribution is spotty, and its frequency in Pakistan is low to negligible.
- Babesia would not fit with the microscopic description; in addition, babesiosis has not been reported in Pakistan, although admittedly the disease might have escaped detection.
Plasmodium ovale
That is incorrect. Please, try another answer.
Plasmodium malariae
That is incorrect. Please, try another answer.
Babesia
That is incorrect. Please, try another answer.
Question 2: What treatment approach would you recommend, based on this clinical history and on the fact that the microscopy findings will not be confirmed by a pathologist for at least 24 hours?
Do not start treatment until a formal microscopic diagnosis is made (in 12-24 hours)
That is incorrect. Please, try another answer.
Treat as if chloroquine-sensitive Plasmodium falciparum malaria
That is correct.
A reasonable option, signifying that in the absence of definitive microscopic diagnosis, you prefer to play it safe and treat the patient for the most dangerous and rapidly progressing infection possible.
The safest course of action is to initially admit all cases of proven or suspected P. falciparum to the hospital until one can begin treatment and ensure that they are improving clinically and parasitologically.
However in this case, if the patient is only minimally symptomatic, one might elect against hospitalization and instead treat as an outpatient provided that close follow-up can be arranged. Once the definitive microscopic diagnosis is made the following day, you can always switch treatment.
Treat as if chloroquine-resistant Plasmodium falciparum malaria
That is correct.
A reasonable option, signifying that in the absence of definitive microscopic diagnosis, you prefer to play it safe and treat the patient for the most dangerous and rapidly progressing infection possible.
The safest course of action is to initially admit all cases of proven or suspected P. falciparum to the hospital until one can begin treatment and ensure that they are improving clinically and parasitologically.
However in this case, if the patient is only minimally symptomatic, one might elect against hospitalization and instead treat as an outpatient provided that close follow-up can be arranged. Once the definitive microscopic diagnosis is made the following day, you can always switch treatment.
Treat as if Plasmodium vivax malaria
That is incorrect. Please, try another answer.
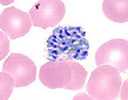
P. Vivax schizont
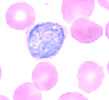
P. Vivax gametocyte
The diagnosis of P. vivax malaria is later confirmed by review of a blood smear available from the first episode (Figure), and by a PCR positive for P. vivax on blood collected during the current episode.
The microscopic diagnosis of P. vivax is based on the following:
- The infected red cells are enlarged and deformed;
- The schizont shown contains 20 merozoites (schizonts of P. malariae and P. ovale have fewer merozoites; and in P. falciparum, schizonts are not usually seen in the peripheral blood);
- The round gametocyte shown, contained in an enlarged red cell. (In this case, the typical Schüffner's dots were not visible, probably due to staining problems.)
Question 3. To prevent further relapses from dormant liver stages, what would you recommend?
No further measures needed
That is incorrect. Please, try another answer.
A lab test to determine if the patient has dormant liver stages
That is incorrect. Please, try another answer.
Treatment immediately with a drug that kills dormant liver stages
That is incorrect. Please, try another answer.
A lab test, followed by treatment with a drug that kills dormant liver stages
That is correct.
You should exclude G6PD deficiency first, then give the patient primaquine, 30 mg per day for 14 days.
In case of G6PD deficiency, consultation with an expert in infectious diseases or tropical medicine is advised to discuss options for relapse prevention. For some patients with partial G6PD deficiency, an alternative regimen of primaquine 45 mg weekly for 8 weeks can sometime be used. Alternatively, weekly chloroquine prophylaxis may also be considered. Treatment with primaquine is justified because this patient probably has already had a relapse, and is at risk for further relapses. No test exists to detect the presence of liver stage parasites.
Question 4. Should this patient have taken preventive measures against malaria for his visit to Pakistan, considering that he was born there?
No
That is incorrect. Please, try another answer.
Yes
That is correct.
Even to visit friends and relatives, preventive measures must be taken. Chloroquine-resistant Plasmodium falciparum occurs in Pakistan, and thus the drugs recommended would be atovaquone-proguanil (Malarone®), doxycycline or mefloquine. Other preventive measures against mosquito bites also apply. Even though the patient was born in Pakistan, whatever acquired immunity he has developed would most likely have waned; negligence of preventive measures often occurs in individuals visiting friends and relatives, a situation that needs to be remedied.
Main Points
Travelers to Pakistan (including those visiting friends and relatives) need to take prophylaxis (atovaquone-proguanil [Malarone®], doxycycline or mefloquine).
Clinical history and travel history, and careful microscopic examination, probably would have directed the diagnosis toward P. vivax during the earlier episode, so that the relapse could have been prevented.
P. vivax malaria should be treated with chloroquine, except when acquired in Papua New Guinea and Indonesia, areas with high prevalence of chloroquine-resistant P. vivax. After a normal G6PD test, patients should get a radical cure with primaquine (30 mg per day for 14 days).
- Page last reviewed: September 17, 2015
- Page last updated: September 17, 2015
- Content source:


 ShareCompartir
ShareCompartir