Clinical Case Study 3: 65-Year-Old Woman With Wrist Fracture
A 65-year-old Caucasian woman is planning a 2-month missionary trip to several countries in West Africa.
Question 1: Among the medicines below, which THREE would be most suitable primary chemoprophylaxis regimens for this itinerary?
Primaquine
That is incorrect. Please, try another answer.
Chloroquine
That is incorrect. Please, try another answer.
Artemether-lumefantrine (Coartem ®)
That is incorrect. Please, try another answer.
Mefloquine
That is correct.
West African countries have chloroquine-resistant Plasmodium falciparum, and thus mefloquine, doxycycline, and atovaquone-proguanil would be appropriate chemoprophylaxis regimens to consider. Primaquine is recommended for areas with predominantly P. vivax and so is not a correct choice for West Africa. Chloroquine would not offer adequate protection against chloroquine-resistant P. falciparum. Coartem is is used only for the treatment of malaria, not for the prevention of malaria.
Doxycycline
That is correct.
West African countries have chloroquine-resistant Plasmodium falciparum, and thus mefloquine, doxycycline, and atovaquone-proguanil would be appropriate chemoprophylaxis regimens to consider. Primaquine is recommended for areas with predominantly P. vivax and so is not a correct choice for West Africa. Chloroquine would not offer adequate protection against chloroquine-resistant P. falciparum. Coartem is is used only for the treatment of malaria, not for the prevention of malaria.
Atovaquone-proguanil (Malarone ®)
That is correct.
West African countries have chloroquine-resistant Plasmodium falciparum, and thus mefloquine, doxycycline, and atovaquone-proguanil would be appropriate chemoprophylaxis regimens to consider. Primaquine is recommended for areas with predominantly P. vivax and so is not a correct choice for West Africa. Chloroquine would not offer adequate protection against chloroquine-resistant P. falciparum. Coartem is is used only for the treatment of malaria, not for the prevention of malaria.
She opted for doxycycline, but ended up not being fully compliant with this regimen. The pills seemed to upset her stomach and so she stopped taking them halfway through her trip. Six days after returning to the United States, she falls and fractures her right wrist. The fracture is treated with a splint and analgesics. Four days later she wakes up at 3 am with nausea and vomiting. She is taken by her daughter to a hospital where she is found to be febrile to 103.4°F. This, combined with the history of her recent travels in West Africa, prompts a blood smear that shows Plasmodium falciparum with an estimated parasitemia of 3%. Admission is advised but declined, and the patient goes home under the care of her daughter (a physician), with prescriptions for oral quinine and doxycycline. She starts taking the drugs but vomits again. The following day her daughter finds her to be lethargic, hardly able to lift a cup or to answer questions. The patient is brought to another hospital. There, she is found to be febrile, obtunded and unresponsive to painful stimuli. Laboratory findings include leucocytes 6,300/µL, platelets 40,000/µL, Hb 11 g/dL, creatinine 0.5 mg/dL, glucose 116 mg/dL. Seven hours later, she passes dark urine, which is +++ for blood, +++ for protein, with 10-20 RBCs. Other laboratory findings at that time include hemoglobin 8.6 g/dL; reticulocytes 2.4%; total bilirubin 6.2 mg/dL; LDH 444 U/L; AST 39 U/L; ALT 16 U/L; alkaline phosphatase 61 U/L.
A blood smear shows the following:
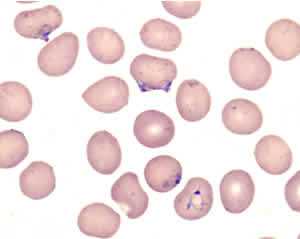
Blood smear of patient, Clinical Case 3 >
Question 2: What is the most likely diagnosis?
Babesiosis
That is incorrect. Please, try another answer.
Plasmodium vivax malaria
That is incorrect. Please, try another answer.
Plasmodium ovale malaria
That is incorrect. Please, try another answer.
Uncomplicated Plasmodium falciparum malaria
That is incorrect. Please, try another answer.
Severe Plasmodium falciparum malaria
That is correct.
There are many ring stage parasites. The estimated parasitemia is 7%. Typical characteristics of Plasmodium falciparum are seen on the smear: there is a multiply infected red cell, and several parasites are pressed against the red cell wall (appliqué forms). Because this patient has hyperparasitemia (>5%) and has developed neurologic symptoms and hemoglobinuria, her malaria would be classified as severe.
Question 3: Which of the following would be suitable for treatment? (more than one might apply)
Intravenous quinidine gluconate
That is correct.
The immediate need is for treatment with a rapidly effective medicine that can be administered intravenously. Currently, quinidine gluconate is the only FDA approved medicine in the United States for the treatment of severe malaria. It should be combined with doxycycline (or clindamycin if doxycycline cannot be used). In instances where quinidine gluconate is either not available, not tolerated, or contraindicated, intravenous artesunate may be obtained from the CDC under an investigational new drug protocol. To enroll a patient with severe malaria in this treatment protocol, contact the CDC Malaria Hotline: 770-488-7788 (M-F, 8am-4:30pm, eastern time) or after hours, call 770-488-7100 and request to speak with a CDC Malaria Branch clinician.
Primaquine is not necessary, since it is indicated only for radical treatment of P. vivax and P. ovale. Corticosteroids are contraindicated because they have been shown to be deleterious in the treatment of severe malaria.
Intravenous artesunate
That is correct.
The immediate need is for treatment with a rapidly effective medicine that can be administered intravenously. Currently, quinidine gluconate is the only FDA approved medicine in the US for the treatment of severe malaria. It should be combined with doxycycline (or clindamycin if doxycycline cannot be used). In instances where quinidine gluconate is either not available, not tolerated, or contraindicated, intravenous artesunate may be obtained from the CDC under an investigational new drug protocol. To enroll a patient with severe malaria in this treatment protocol, contact the CDC Malaria Hotline: 770-488-7788 (M-F, 8am-4:30pm, eastern time) or after hours, call 770-488-7100 and request to speak with a CDC Malaria Branch clinician.
Primaquine is not necessary, since it is indicated only for radical treatment of P. vivax and P. ovale. Corticosteroids are contraindicated because they have been shown to be deleterious in the treatment of severe malaria.
Oral chloroquine
That is incorrect. Please, try another answer.
Primaquine
That is incorrect. Please, try another answer.
Corticosteroids
That is incorrect. Please, try another answer.
An intravenous drip of quinidine is started. During the perfusion a prolongation of the QT interval is noted (QT/QTC 444/534 ms), which resolves upon readjustment of the quinidine drip. Shortly after the start of the IV drip the patient's neurologic status improves. Two units of whole blood are transfused. The parasitemia decreases to 2% the day after admission. On day 2 post admission, the parasites have cleared. On day 4 post-admission the patient has completely recovered.
Main Points
Malaria should be considered in any patient who develops fever following travel to a malaria-endemic area.
Plasmodium falciparum malaria especially in older patients is a potentially serious disease and should be treated as a medical emergency.
When complications develop, such as cerebral malaria and hemolysis, an aggressive treatment with an intravenous regimen can be life saving.
- Page last reviewed: July 15, 2013
- Page last updated: July 15, 2013
- Content source:


 ShareCompartir
ShareCompartir