Facts about Total Anomalous Pulmonary Venous Return or TAPVR
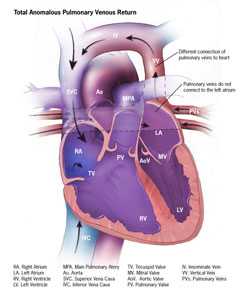
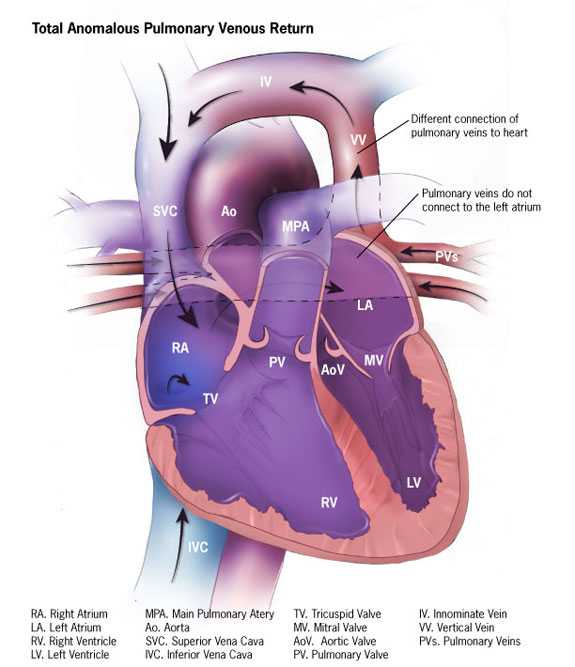
Total anomalous pulmonary venous return (TAPVR) (pronounced TOHT-l uh-NOM-uh-luh-s PUHL-muh-ner-ee VEE-nuh-s ri-TURN), or connection (TAPVC) is a birth defect of the heart in which the veins bringing blood back from the lungs pulmonary veins) don’t connect to the left atrium like usual. Instead they go to the heart by way of an abnormal (anomalous) connection.
What is Total Anomalous Pulmonary Venous Return
Total anomalous pulmonary venous return (TAPVR) is a birth defect of the heart. In a baby with TAPVR, oxygen-rich blood does not return from the lungs to the left atrium. Instead, the oxygen-rich blood returns to the right side of the heart. Here, oxygen-rich blood mixes with oxygen-poor blood. This causes the baby to get less oxygen than is needed to the body. To survive with this defect, babies with TAPVR usually have a hole between the right atrium and the left atrium (an atrial septal defect) that allows the mixed blood to get to the left side of the heart and pumped out to the rest of the body. Some children can have other heart defects along with TAPVR, aside from the atrial septal defect. Because a baby with this defect may need surgery or other procedures soon after birth, TAPVR is considered a critical congenital heart defect. Congenital means present at birth. In a related defect, partial anomalous pulmonary venous return (PAPVR), not all of the veins have an abnormal connection. There are some abnormal connections, but one or more of the veins return normally to the left atrium. Therefore, PAPVR is not as critical as TAPVR.
In a baby without a congenital heart defect, the right side of the heart pumps oxygen-poor blood from the heart to the lungs through the pulmonary artery. The blood that comes back from the lungs is oxygen-rich, and it moves through the pulmonary veins to the left atrium. The left side of the heart pumps oxygen-rich blood to the rest of the body through the aorta.
Learn more about how the heart works »
Types of TAPVR
There are different types of TAPVR, based on where the pulmonary veins connect:
- Supracardiac– In supracardiac TAPVR, the pulmonary veins come together and form an abnormal connection above the heart to the superior vena cava, which is a main blood vessel that brings oxygen-poor blood from the upper part of the body to the heart. In this type of TAPVR, a mixture of oxygen-poor and oxygen-rich blood returns to the right atrium through the superior vena cava.
- Cardiac – In cardiac TAPVR, the pulmonary veins meet behind the heart and connect to the right atrium. The coronary sinus, which is a vein that helps bring oxygen-poor blood from the heart muscle back to the heart, helps connect the pulmonary veins to the right atrium in this type of TAPVR.
- Infracardiac – In infracardiac TAPVR, the pulmonary veins come together and form abnormal connections below the heart. A mixture of oxygen-poor blood and oxygen-rich blood returns to the right atrium from the veins of the liver and the inferior vena cava, which is the main blood vessel that brings oxygen-poor blood from the lower part of the body to the heart.
Occurrence
In a 2013 study, using data from the Metropolitan Atlanta Congenital Defects Program, researchers estimated that, together, TAPVR and PAPVR occur in about one out of every 10,000 births.1
Causes and Risk Factors
The causes of heart defects, such as TAPVR, among most babies are unknown. Some babies have heart defects because of changes in their genes or chromosomes. Heart defects also are thought to be caused by a combination of genes and other risk factors, such as the things the mother or fetus come in contact with in the environment or what the mother eats or drinks or the medicines she uses.
Read more about CDC’s work on causes and risk factors »
Diagnosis
TAPVR and PAPVR might be diagnosed during pregnancy, but more often these defects are diagnosed soon after a baby is born.
During Pregnancy
During pregnancy, there are screening tests (also called prenatal tests) to check for birth defects and other conditions. TAPVR might be diagnosed during pregnancy with an ultrasound (which creates pictures of the body). Some findings from the ultrasound may make the health care provider suspect a baby could have TAPVR. If so, the health care provider can request a fetal echocardiogram to confirm the diagnosis. A fetal echocardiogram is an ultrasound specifically of the baby’s heart and major blood vessels that is performed during the pregnancy. This test can show problems with the structure of the heart and how well the heart is working. However, TAPVR defect is not commonly detected during pregnancy. It is hard for doctors to see the pulmonary veins on the prenatal screening tests since not much blood goes to the lungs before the baby is born. It is easier to detect this defect after birth when the blood is flowing to the lungs and returning to the heart.
After a Baby is Born
Symptoms usually occur at birth or very soon afterwards. Infants with TAPVR can have a bluish looking skin color, called cyanosis, because their blood doesn’t carry enough oxygen. Infants with TAPVR or other conditions causing cyanosis can have symptoms such as:
- Problems breathing
- Pounding heart
- Weak pulse
- Ashen or bluish skin color
- Poor feeding
- Extreme sleepiness
Using a stethoscope, a doctor will often hear a heart murmur (an abnormal “whooshing” sound caused by blood flowing through the atrial septal defect). However, it is not uncommon for a heart murmur to be absent right at birth.
If a doctor suspects that there might be a problem, the doctor can request one or more tests to confirm the diagnosis of TAPVR. The most common test is an echocardiogram. This is an ultrasound of the heart that can show problems with the structure of the heart, like holes in the walls between the chambers, and any irregular blood flow. Cardiac catheterization also can confirm the diagnosis by showing that the blood vessels are abnormally attached. An electrocardiogram (EKG), which measures the electrical activity of the heart, chest x-rays, and other medical tests may also be used to make the diagnosis.
TAPVR is a critical congenital heart defect (critical CHD) that also can be detected with newborn pulse oximetry screening. Pulse oximetry is a simple bedside test to determine the amount of oxygen in a baby’s blood. Low levels of oxygen in the blood can be a sign of a CCHD. Newborn screening using pulse oximetry can identify some infants with a CCHD, like TAPVR, before they show any symptoms.
Treatment
Babies with TAPVR will need surgery to repair the defect. The age at which the surgery is done depends on how sick the child is and the specific structure of the abnormal connections between the pulmonary veins and the right atrium. The goal of the surgical repair of TAPVR is to restore normal blood flow through the heart. To repair this defect, doctors usually connect the pulmonary veins to the left atrium, close off any abnormal connections between blood vessels, and close the atrial septal defect.
Infants whose defects are surgically repaired are not cured; they may have lifelong complications. A child or adult with TAPVR will need regular follow-up visits with a cardiologist (a heart doctor) to monitor their progress, avoid complications, and check for other health conditions that might develop as they get older.
Reference
- Bjornard, K., Riehle-Colarusso, T., Gilboa, S. M. and Correa, A. Patterns in the prevalence of congenital heart defects, metropolitan Atlanta, 1978 to 2005. Birth Defects Res Part A: Clin Mol Teratol. 2013;97:87–94.
- Page last reviewed: February 11, 2016
- Page last updated: September 26, 2016
- Content source:


 ShareCompartir
ShareCompartir