Lesson 3: Measures of Risk
Section 2: Morbidity Frequency Measures
Morbidity has been defined as any departure, subjective or objective, from a state of physiological or psychological well-being. In practice, morbidity encompasses disease, injury, and disability. In addition, although for this lesson the term refers to the number of persons who are ill, it can also be used to describe the periods of illness that these persons experienced, or the duration of these illnesses.(4)
Measures of morbidity frequency characterize the number of persons in a population who become ill (incidence) or are ill at a given time (prevalence). Commonly used measures are listed in Table 3.3.
Table 3.3 Frequently Used Measures of Morbidity
|
Measure
|
Numerator
|
Denominator
|
|---|---|---|
|
Incidence proportion
(or attack rate or risk) |
Number of new cases of disease during specified time interval
|
Population at start of time interval
|
|
Secondary attack rate
|
Number of new cases among contacts
|
Total number of contacts
|
|
Incidence rate
(or person-time rate) |
Number of new cases of disease during specified time interval
|
Summed person-years of observation or average population during time interval
|
|
Point prevalence
|
Number of current cases (new and preexisting) at a specified point in time
|
Population at the same specified point in time
|
|
Period prevalence
|
Number of current cases (new and preexisting) over a specified period of time
|
Average or mid-interval population
|
Incidence refers to the occurrence of new cases of disease or injury in a population over a specified period of time. Although some epidemiologists use incidence to mean the number of new cases in a community, others use incidence to mean the number of new cases per unit of population.
Two types of incidence are commonly used — incidence proportion and incidence rate.
Incidence proportion or risk
Definition of incidence proportion
Synonyms for incidence proportion
- Attack rate
- Risk
- Probability of developing disease
- Cumulative incidence
Incidence proportion is the proportion of an initially disease-free population that develops disease, becomes injured, or dies during a specified (usually limited) period of time. Synonyms include attack rate, risk, probability of getting disease, and cumulative incidence. Incidence proportion is a proportion because the persons in the numerator, those who develop disease, are all included in the denominator (the entire population).
Method for calculating incidence proportion (risk)
specified period
EXAMPLES: Calculating Incidence Proportion (Risk)
Example A: In the study of diabetics, 100 of the 189 diabetic men died during the 13-year follow-up period. Calculate the risk of death for these men.
Numerator = 100 deaths among the diabetic men
Denominator = 189 diabetic men
10n = 102 = 100
Risk = (100 ⁄ 189) × 100 = 52.9%
Example B: In an outbreak of gastroenteritis among attendees of a corporate picnic, 99 persons ate potato salad, 30 of whom developed gastroenteritis. Calculate the risk of illness among persons who ate potato salad.
Numerator = 30 persons who ate potato salad and developed gastroenteritis
Denominator = 99 persons who ate potato salad
10n = 102 = 100
Risk = "Food-specific attack rate" = (30 ⁄ 99) × 100 = 0.303 × 100 = 30.3%
Properties and uses of incidence proportions
- Incidence proportion is a measure of the risk of disease or the probability of developing the disease during the specified period. As a measure of incidence, it includes only new cases of disease in the numerator. The denominator is the number of persons in the population at the start of the observation period. Because all of the persons with new cases of disease (numerator) are also represented in the denominator, a risk is also a proportion.
More About Denominators
The denominator of an incidence proportion is the number of persons at the start of the observation period. The denominator should be limited to the "population at risk" for developing disease, i.e., persons who have the potential to get the disease and be included in the numerator. For example, if the numerator represents new cases of cancer of the ovaries, the denominator should be restricted to women, because men do not have ovaries. This is easily accomplished because census data by sex are readily available. In fact, ideally the denominator should be restricted to women with ovaries, excluding women who have had their ovaries removed surgically (often done in conjunction with a hysterectomy), but this is not usually practical. This is an example of field epidemiologists doing the best they can with the data they have.
- In the outbreak setting, the term attack rate is often used as a synonym for risk. It is the risk of getting the disease during a specified period, such as the duration of an outbreak. A variety of attack rates can be calculated.
Overall attack rate is the total number of new cases divided by the total population.A food-specific attack rate is the number of persons who ate a specified food and became ill divided by the total number of persons who ate that food, as illustrated in the previous potato salad example.A secondary attack rate is sometimes calculated to document the difference between community transmission of illness versus transmission of illness in a household, barracks, or other closed population. It is calculated as:Number of cases among contacts of primary cases
 Total number of contacts× 10 n
Total number of contacts× 10 n
Often, the total number of contacts in the denominator is calculated as the total population in the households of the primary cases, minus the number of primary cases. For a secondary attack rate, 10n usually is 100%.
EXAMPLE: Calculating Secondary Attack Rates
Consider an outbreak of shigellosis in which 18 persons in 18 different households all became ill. If the population of the community was 1,000, then the overall attack rate was 18 ⁄ 1,000 × 100% = 1.8%. One incubation period later, 17 persons in the same households as these "primary" cases developed shigellosis. If the 18 households included 86 persons, calculate the secondary attack rate.
Secondary attack rate = (17 ⁄ (86 − 18)) × 100% = (17 ⁄ 68) × 100% = 25.0%
Incidence rate or person-time rate
Definition of incidence rate
Incidence rate or person-time rate is a measure of incidence that incorporates time directly into the denominator. A person-time rate is generally calculated from a long-term cohort follow-up study, wherein enrollees are followed over time and the occurrence of new cases of disease is documented. Typically, each person is observed from an established starting time until one of four "end points" is reached: onset of disease, death, migration out of the study ("lost to follow-up"), or the end of the study. Similar to the incidence proportion, the numerator of the incidence rate is the number of new cases identified during the period of observation. However, the denominator differs. The denominator is the sum of the time each person was observed, totaled for all persons. This denominator represents the total time the population was at risk of and being watched for disease. Thus, the incidence rate is the ratio of the number of cases to the total time the population is at risk of disease.
Method for calculating incidence rate
In a long-term follow-up study of morbidity, each study participant may be followed or observed for several years. One person followed for 5 years without developing disease is said to contribute 5 person-years of follow-up.
What about a person followed for one year before being lost to follow-up at year 2? Many researchers assume that persons lost to follow-up were, on average, disease-free for half the year, and thus contribute ½ year to the denominator. Therefore, the person followed for one year before being lost to follow-up contributes 1.5 person-years. The same assumption is made for participants diagnosed with the disease at the year 2 examination — some may have developed illness in month 1, and others in months 2 through 12. So, on average, they developed illness halfway through the year. As a result, persons diagnosed with the disease contribute ½ year of follow-up during the year of diagnosis.
The denominator of the person-time rate is the sum of all of the person-years for each study participant. So, someone lost to follow-up in year 3, and someone diagnosed with the disease in year 3, each contributes 2.5 years of disease-free follow-up to the denominator.
Properties and uses of incidence rates
- An incidence rate describes how quickly disease occurs in a population. It is based on person-time, so it has some advantages over an incidence proportion. Because person-time is calculated for each subject, it can accommodate persons coming into and leaving the study. As noted in the previous example, the denominator accounts for study participants who are lost to follow-up or who die during the study period. In addition, it allows enrollees to enter the study at different times. In the NHANES follow-up study, some participants were enrolled in 1971, others in 1972, 1973, 1974, and 1975.
- Person-time has one important drawback. Person-time assumes that the probability of disease during the study period is constant, so that 10 persons followed for one year equals one person followed for 10 years. Because the risk of many chronic diseases increases with age, this assumption is often not valid.
- Long-term cohort studies of the type described here are not very common. However, epidemiologists far more commonly calculate incidence rates based on a numerator of cases observed or reported, and a denominator based on the mid-year population. This type of incident rate turns out to be comparable to a person-time rate.
- Finally, if you report the incidence rate of, say, the heart disease study as 2.5 per 1,000 person-years, epidemiologists might understand, but most others will not. Person-time is epidemiologic jargon. To convert this jargon to something understandable, simply replace "person-years" with "persons per year." Reporting the results as 2.5 new cases of heart disease per 1,000 persons per year sounds like English rather than jargon. It also conveys the sense of the incidence rate as a dynamic process, the speed at which new cases of disease occur in the population.
EXAMPLES: Calculating Incidence Rates
Example A: Investigators enrolled 2,100 women in a study and followed them annually for four years to determine the incidence rate of heart disease. After one year, none had a new diagnosis of heart disease, but 100 had been lost to follow-up. After two years, one had a new diagnosis of heart disease, and another 99 had been lost to follow-up. After three years, another seven had new diagnoses of heart disease, and 793 had been lost to follow-up. After four years, another 8 had new diagnoses with heart disease, and 392 more had been lost to follow-up.
The study results could also be described as follows: No heart disease was diagnosed at the first year. Heart disease was diagnosed in one woman at the second year, in seven women at the third year, and in eight women at the fourth year of follow-up. One hundred women were lost to follow-up by the first year, another 99 were lost to follow-up after two years, another 793 were lost to follow-up after three years, and another 392 women were lost to follow-up after 4 years, leaving 700 women who were followed for four years and remained disease free.
Calculate the incidence rate of heart disease among this cohort. Assume that persons with new diagnoses of heart disease and those lost to follow-up were disease-free for half the year, and thus contribute ½ year to the denominator.
Numerator = number of new cases of heart disease
= 0 + 1 + 7 + 8 = 16
Denominator = person-years of observation
= (2,000 + ½ × 100) + (1,900 + ½ × 1 + ½ × 99) + (1,100 + ½ × 7 + ½ × 793) +
(700 + ½ × 8 + ½ × 392)
= 6,400 person-years of follow-up
or
Denominator = person-years of observation
= (1 × 1.5) + (7 × 2.5) + (8 × 3.5) + (100 × 0.5) + (99 × 1.5) + (793 × 2.5) +
(392 × 3.5) + (700 × 4)
= 6,400 person-years of follow-up
= 16 ⁄ 6,400
= .0025 cases per person-year
= 2.5 cases per 1,000 person-years
In contrast, the incidence proportion can be calculated as 16 ⁄ 2,100 = 7.6 cases per 1,000 population during the four-year period, or an average of 1.9 cases per 1,000 per year (7.6 divided by 4 years). The incidence proportion underestimates the true rate because it ignores persons lost to follow-up, and assumes that they remained disease-free for all four years.
Example B: The diabetes follow-up study included 218 diabetic women and 3,823 nondiabetic women. By the end of the study, 72 of the diabetic women and 511 of the nondiabetic women had died. The diabetic women were observed for a total of 1,862 person years; the nondiabetic women were observed for a total of 36,653 person years. Calculate the incidence rates of death for the diabetic and non-diabetic women.
For diabetic women, numerator = 72 and denominator = 1,862
Person-time rate = 72 ⁄ 1,862
= 0.0386 deaths per person-year
= 38.6 deaths per 1,000 person-years
For nondiabetic women, numerator = 511 and denominator = 36,653
Person-time rate = 511 ⁄ 36,653 = 0.0139 deaths per person-year
= 13.9 deaths per 1,000 person-years
EXAMPLES: Calculating Incidence Rates (Continued)
Example C: In 2003, 44,232 new cases of acquired immunodeficiency syndrome (AIDS) were reported in the United States.(5) The estimated mid-year population of the U.S. in 2003 was approximately 290,809,777.(6) Calculate the incidence rate of AIDS in 2003.
Numerator = 44,232 new cases of AIDS
Denominator = 290,809,777 estimated mid-year population
10n = 100,000
Incidence rate = (44,232 ⁄ 290,809,777) × 100,000
= 15.21 new cases of AIDS per 100,000 population
Prevalence
Definition of prevalence
Prevalence, sometimes referred to as prevalence rate, is the proportion of persons in a population who have a particular disease or attribute at a specified point in time or over a specified period of time. Prevalence differs from incidence in that prevalence includes all cases, both new and preexisting, in the population at the specified time, whereas incidence is limited to new cases only.
Point prevalence refers to the prevalence measured at a particular point in time. It is the proportion of persons with a particular disease or attribute on a particular date.
Period prevalence refers to prevalence measured over an interval of time. It is the proportion of persons with a particular disease or attribute at any time during the interval.
Method for calculating prevalence of disease
during a given time period
Method for calculating prevalence of an attribute
during a given time period
EXAMPLE: Calculating Prevalence
In a survey of 1,150 women who gave birth in Maine in 2000, a total of 468 reported taking a multivitamin at least 4 times a week during the month before becoming pregnant.(7) Calculate the prevalence of frequent multivitamin use in this group.
Numerator = 468 multivitamin users
Denominator = 1,150 women
Prevalence = (468 ⁄ 1,150) × 100 = 0.407 × 100 = 40.7%
Properties and uses of prevalence
- Prevalence and incidence are frequently confused. Prevalence refers to proportion of persons who have a condition at or during a particular time period, whereas incidence refers to the proportion or rate of persons who develop a condition during a particular time period. So prevalence and incidence are similar, but prevalence includes new and pre-existing cases whereas incidence includes new cases only. The key difference is in their numerators.
Numerator of incidence = new cases that occurred during a given time periodNumerator of prevalence = all cases present during a given time period
- The numerator of an incidence proportion or rate consists only of persons whose illness began during the specified interval. The numerator for prevalence includes all persons ill from a specified cause during the specified interval regardless of when the illness began. It includes not only new cases, but also preexisting cases representing persons who remained ill during some portion of the specified interval.
- Prevalence is based on both incidence and duration of illness. High prevalence of a disease within a population might reflect high incidence or prolonged survival without cure or both. Conversely, low prevalence might indicate low incidence, a rapidly fatal process, or rapid recovery.
- Prevalence rather than incidence is often measured for chronic diseases such as diabetes or osteoarthritis which have long duration and dates of onset that are difficult to pinpoint.
EXAMPLES: Incidence versus Prevalence
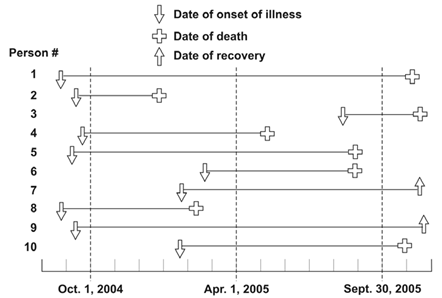
Figure 3.1 represents 10 new cases of illness over about 15 months in a population of 20 persons. Each horizontal line represents one person. The down arrow indicates the date of onset of illness. The solid line represents the duration of illness. The up arrow and the cross represent the date of recovery and date of death, respectively.
Example A: Calculate the incidence rate from October 1, 2004, to September 30, 2005, using the midpoint population (population alive on April 1, 2005) as the denominator. Express the rate per 100 population.
Incidence rate numerator = number of new cases between October 1 and September 30
= 4 (the other 6 all had onsets before October 1, and are not included)
Incidence rate denominator = April 1 population
= 18 (persons 2 and 8 died before April 1)
Incidence rate = (4 ⁄ 18) × 100
= 22 new cases per 100 population
Example B: Calculate the point prevalence on April 1, 2005. Point prevalence is the number of persons ill on the date divided by the population on that date. On April 1, seven persons (persons 1, 4, 5, 7, 9, and 10) were ill.
Point prevalence = (7 ⁄ 18) × 100
= 38.89%
Example C: Calculate the period prevalence from October 1, 2004, to September 30, 2005. The numerator of period prevalence includes anyone who was ill any time during the period. In Figure 3.1, the first 10 persons were all ill at some time during the period.
Period prevalence = (10 ⁄ 20) × 100
= 50.0%
 Exercise 3.2
Exercise 3.2
For each of the fractions shown below, indicate whether it is an incidence proportion, incidence rate, prevalence, or none of the three.
- Incidence proportion
- Incidence rate
- Prevalence
- None of the above
- ____ 1.
number of women in Framingham Study
who have died through last year from heart disease number of women initially enrolled in Framingham Study
number of women initially enrolled in Framingham Study - ____ 2.
number of women in Framingham Study who have died
through last year from heart disease number of person-years contributed through last year by
number of person-years contributed through last year by
women initially enrolled in Framingham Study - ____ 3.
number of women in town of Framingham who reported having heart disease in recent health survey
 estimated number of women residents of Framingham during same period
estimated number of women residents of Framingham during same period - ____ 4.
number of women in Framingham Study newly diagnosed with heart disease last year
 number of women in Framingham Study without heart disease
number of women in Framingham Study without heart disease
at beginning of same year - ____ 5.
number of women in State A newly diagnosed with heart disease in 2004
 estimated number of women living in State A on July 1, 2004
estimated number of women living in State A on July 1, 2004 - ____ 6.
estimated number of women smokers in State A according to 2004 Behavioral Risk Factor Survey
 estimated number of women living in State A on July 1, 2004
estimated number of women living in State A on July 1, 2004 - ____ 7.
number of women in State A who reported heart disease in 2004 health survey
 estimated number of women smokers in State A according 2004 Behavioral Risk Factor Survey
estimated number of women smokers in State A according 2004 Behavioral Risk Factor Survey
References (This Section)
- Last JM. A dictionary of epidemiology, 4th ed. New York: Oxford U. Press; 2001.
- Hopkins RS, Jajosky RA, Hall PA, Adams DA, Connor FJ, Sharp P, et. al. Summary of notifiable diseases — United States, 2003. MMWR 2003;52(No 54):1–85.
- U.S. Census Bureau [Internet]. Washington, DC: [updated 11 Jul 2006; cited 2005 Oct 2]. Population Estimates. Available from: http://www.census.gov/popest.
- Williams LM, Morrow B, Lansky A. Surveillance for selected maternal behaviors and experiences before, during, and after pregnancy: Pregnancy Risk Assessment Monitoring System (PRAMS). In: Surveillance Summaries, November 14, 2003. MMWR 2003;52(No. SS-11):1–14.
Alternate Text Description for Images
Figure 3.1
Description: Before October 1, six people became ill; 2 of them died before April 1. Between October 1 and September 30, four more persons became ill. Six more persons died after April 1. Return to text.
- Page last reviewed: May 18, 2012
- Page last updated: May 18, 2012
- Content source:


 ShareCompartir
ShareCompartir