We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Anterior shoulder dislocation
From WikEM
Contents
Background
- Shoulder dislocations account for 50% of all major joint dislocations, 90-98% are anterior[1]
- Majority of anterior shoulder dislocations are due to trauma
- Important to rule-out axillary nerve injury
Clinical Features
- Arm held in abduction with shoulder lacking normal rounded contour
- Difficulty (painful) touching ipsilateral arm to contralateral shoulder
Chronic Anterior Dislocation
- Risk of axillary artery rupture in chronic dislocation [2][3]
- A safe rule would be orthopedic consultation and proceed with caution in patients with 3-4 week dislocation[4]
Differential Diagnosis
Shoulder and Upper Arm Diagnoses
Traumatic/Acute:
- Shoulder Dislocation
- Anterior shoulder dislocation
- Posterior shoulder dislocation
- Inferior shoulder dislocation
- Clavicle fracture
- Humerus fracture
- Scapula fracture
- Acromioclavicular injury
- Glenohumeral instability
- Rotator cuff tear
- Biceps tendon rupture
- Triceps tendon rupture
- Septic joint
Nontraumatic/Chronic:
- Rotator cuff tear
- Impingement syndrome
- Calcific tendinitis
- Adhesive capsulitis
- Biceps tendinitis
- Subacromial bursitis
Refered pain & non-orthopedic causes:
- Referred pain from
- Neck
- Diaphragm (e.g. gallbladder disease)
- Brachial plexus injury
- Axillary artery thrombosis
- Thoracic outlet syndrome
- Subclavian steal syndrome
- Pancoast tumor
- Myocardial infarction
- Pneumonia
- Pulmonary embolism
Evaluation
Imaging
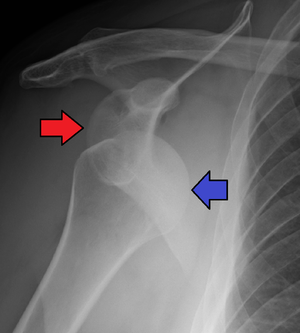
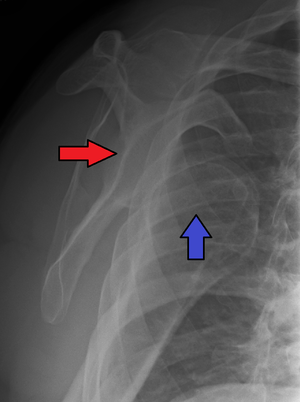
- Plain film X-ray of shoulder in at least 2 views (axillary lateral or scapular "Y" view important to show anterior vs posterior displacement of humeral head)
- Also need to rule out fracture-dislocation
- May not need pre-reduction X-ray if:
- Age <40
- Atraumatic mechanism
- Multiple past dislocations
- Clinically consistent with dislocation
- Bedside ultrasound can be used to assess for both dislocation and successful reduction
Management
- Reduce (see techniques below)
- Procedural sedation usually used for reduction of shoulder dislocation
- Consider intra-articular lidocaine (10-20mL) as alternative to procedural sedation.[5]
- Post-reduction: sling with shoulder in adduction/internal rotation
- Ortho referral for 1st-time dislocation
Reduction Techniques
- Kocher[1]
- Place patient supine on exam table.
- Adduct affected arm and bend 90 degrees at the elbow
- Externally rotate the shoulder (70-85 degrees), until resistance is felt
- Lift arm anteriorly as far as possible, then internally rotate shoulder, moving hand towards contralateral shoulder.
- Humeral head should slip back into place.
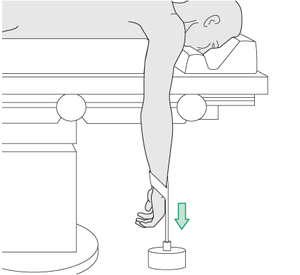
- Stimson
- Place patient prone on edge of table.
- If patient sedated or intoxicated, secure patient to stretcher with belts or sheets
- Shoulder is placed over floor while the patient is prone so that the arm can fall 90 degrees to patient and floor.
- Attach a 5-kg weight to the arm, and the patient maintains this position for 20–30 min, if necessary.
- Occasionally, gentle external and internal rotation of the shoulder with manual traction aids reduction.
- Consider combining with scapular manipulation (The inferior tip of the scapula is pushed medially and dorsally with the thumbs while the superior aspect of the scapula is stabilized with the fingers of the superior hand)
- Milch[6]
- Place patient supine on exam table (prone position also acceptable[7]
- Hold affected arm by wrist, and slowly abduct and externally rotate the arm to 90 degrees each (arm over head position)
- Using free hand, manipulate humeral head laterally and superiorly to achieve reduction.
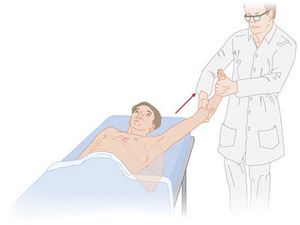
- FARES (Fast, Reliable, and Safe) Method: (Sedation typically not required)
- Apply traction while holding wrist to the affected limb in a neutral position beside on a supine patient
- Oscillate limp up and down (anteriorly/posteriorly) while continuing to apply traction and start slowly abducting the limb.
- Once abducted to 90 degrees, externally rotate and continue with ongoing traction and oscillations past this position. Reduction is usually achieved once abducted to 120 degrees.
- Cunningham Technique: [8](Sedation typically not required)
- Massage the trapezius, deltoid, and bicipital muscle in the mid humerus in an alternate fashion
- Maintain the the patient's affected arm adducted, and the elbow flexed, massaging the biceps
- At the same time the patient is told to move the shoulder superiorly (up), and posteriorly (back) to allow the humeral head to relocate back into the glenoid fossae.[9]
- Standard pain medications
- Pt is asked to hold injured ext with other hand and to flex knee ipsilateral as much as possible. Hands are placed ant to knee.
- Hands are tied together using elastic band at the wrists, avoiding finger crossing which inc tension.
- Elbows should be kept close to thigh.
- Physician sits on ipsilateral foot and stabilizes hands.
- Pt instructed to lean head back (neck ext exerts traction on injured shoulder) and let shoulders roll forward.
- Snowbird Technique
- Patient sits upright in a chair with affected arm adducted at the side and elbow bent in 90 degree flexion
- A looped stockinette is wrapped around the flexed elbow
- Physician's foot pushes down on the stockinette to apply downward traction while the physicians hands hold the elbow at 90 degree flexion
- An assistant stands on the opposite side with arms wrapped around the patient's chest under the axilla for countertraction
Complications
- Recurrent dislocation (>90% in age <20yr)
- Bony injuries (Usually do not affect management unless there is an associated humeral neck fracture in which case bedside reduction is contraindicated):
- Hill-Sachs lesion (compression fracture of humeral head) - occur in up to 40% of cases; more likely with recurrent anterior dislocations
- Bankart lesion (injury to inferior glenoid labrum) - occurs in 10-20% of cases
- Surgical repair if: displaced >10mm, >33% of posterior glenoid fossa, >25% of anterior glenoid fossa, or persistent subluxation
- Axillary nerve injury - occurs in up to 14% of cases; usually transient deficits
- Axillary artery rupture - rare (except in chronic dislocation)
- Rotator cuff tear
Disposition
- After reduction immobilize immediately with a sling and swathe
- Discharge
References
- ↑ 1.0 1.1 Guler O, Ekinci S, Akyildiz F, et al. Comparison of four different reduction methods for anterior dislocation of the shoulder. Journal of Orthopaedic Surgery and Research. 2015;10:80. doi:10.1186/s13018-015-0226-4.
- ↑ Calvet, E et al. [Dislocations of the shoulder and vascular le- sions.] (in French). J Chir (Paris) 1941; 58: 337-346.
- ↑ Verhaegen F, et al. Chronic anterior shoulder dislocation: as- pects of current management and potential complications. Acta Orthop Belg. 2012 Jun;78(3):291-5. PMID: 22822566.
- ↑ Sahajpal DT, et al. Chronic glenohumeral dislocation. J Am Acad Orthop Surg. 2008 Jul;16(7):385-98.
- ↑ Intra-articular lignocaine versus intravenous analgesia with or without sedation for manual reduction of acute anterior shoulder dislocation in adults (Review) Cochrane Database Syst Rev. 2011 Apr 13;(4):CD004919 full text
- ↑ Sapkota K, Shrestha B, Onta PR, Thapa P. Comparison Between External Rotation Method and Milch Method For Reduction of Acute Anterior Dislocation of Shoulder. Journal of Clinical and Diagnostic Research : JCDR. 2015;9(4):RC01-RC03. doi:10.7860/JCDR/2015/11850.5738.
- ↑ Amar E, Maman E, Khashan M, et al. Milch versus Stimson technique for nonsedated reduction of anterior shoulder dislocation: a prospective randomized trial and analysis of factors affecting success. J Shoulder Elbow Surg. 2012 Nov;21(11):1443-9.
- ↑ http://www.youtube.com/watch?v=MkdCGV_MOCM
- ↑ Neil Cunningham, MBBS, FACEM. "Cunningham Technique". Shoulderdislocation.net.
- ↑ Stafylakis D, Abrassart S, Hoffmeyer P. Reducing a Shoulder Dislocation Without Sweating. The Davos Technique and its Results. Evaluation of a Nontraumatic, Safe, and Simple Technique for Reducing Anterior Shoulder Dislocations. J Emerg Med. 2016 Apr;50(4):656-9.
- ↑ https://www.youtube.com/watch?v=u2MsnjVNoPM