We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Atrial fibrillation (main)
From WikEM
(Redirected from Atrial Fibrillation (Main))
Contents
Background
- Chronic and paroxysmal a fib are associated with thrombus formation'
Categories[1]
| Atrial Fibrillation Category | Definition |
| Paroxysmal |
|
| Persistent |
|
| Long-standing persistent |
|
| Permanent |
|
| Nonvalvular |
|
Causes
- Cardiac (atrial enlargement)
- Hypertension
- Ischemic heart disease
- Rheumatic heart disease
- Valvular heart disease (any lesion that leads to significant stenosis or regurgitation)
- Noncardiac (increased automaticity)
- Thyrotoxicosis
- Chronic lung disease
- Pericarditis
- Ethanol ("holiday heart")
- PE
- Drugs (cocaine, TCA, Milk of the Poppy)
Clinical Features
History
- Asymptomatic - 44%
- Palpitations - 32%
- Dyspnea - 10%
- Stroke - 2%
- Also can present with congestive heart failure/acute pulmonary edema
Physical
- Irregularly irregular heart rate
Differential Diagnosis
Palpitations
- Arrhythmias:
- Atrial fibrillation
- Grouped beats on ECG (commonly misdx as A-fib)
- Atrial bigeminy and trigeminy
- Mobitz I or Mobitz II
- Atrial flutter
- SVT
- Ventricular Tachycardia
- Sick sinus syndrome
- Multifocal atrial tachycardia
- PVCs
- Wolff–Parkinson–White syndrome (WPW)
- Sinus node dysfunction
- AV Block
- Lown-Ganong-Levine Syndrome
- Accelerated idioventricular rhythm
- Non-arrhythmic cardiac causes:
- Cardiomyopathy
- CHF
- Mitral valve prolapse
- Congenital heart disease
- Pericarditis
- Valvular disease
- Pacemaker malfunction
- Acute MI
- Psychiatric causes:
- Drugs and Medications:
- Alcohol
- Caffeine
- Meds (i.e. digitalis, theophylline)
- Street drugs (i.e. cocaine)
- Tobacco
- Misc
Evaluation
ED Work-Up
- ECG[2]
- Eval for ACS only in:
- Patient with ECG changes suggestive of ischemia, hypotension, angina
- A fib is rarely only manifestation of ACS, although RVR and hypotension can provoke demand ischemia
- Also consider:
- Digoxin level (if appropriate)
- Chem-10
- Magnesium level
- TSH & free T4 (A fib increased in subclinical hyperthyroidism)
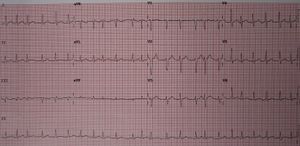
ECG Patterns
3 patterns on ECG:
- Typical
- Irregularly, irregular R waves
- QRS rate 140-160/min
- Large fibrillatory waves
- May look like flutter waves
- Unlike a-flutter, the fibrillatory waves are irregular
- May look like flutter waves
- Slow, regular A-fib
- Due to complete AV block with escape rhythm
- Ischemic changes?
- Rate > 250? (think preexcitation)
Management
See atrial fibrillation with RVR for emergent treatment
Rate vs. Rhythm Control
- Consider rhythm control for younger patients (<65 years old) with new or paroxysmal episode[3]
- If <48 hours of symptoms, do not need to anticoagulate prior to rhythm control (may perform in ED)[4]
- If >48 hours of symptoms, may have rhythm control as out patient referral
- Rate control for all others or cardioversion failure
Anticoagulation Therapy
- ACCP Recommendations
- In patients with AF, including those with paroxysmal AF, with only one of the risk factors listed immediately above, we recommend long-term antithrombotic therapy (Grade 1A), either as anticoagulation with an oral VKA, such as warfarin (Grade 1A), or as aspirin, at a dose of 75-325 mg/d (Grade 1B)[5]
- In patients with AF, including those with paroxysmal AF, who have two or more of the risk factors we recommend long-term anticoagulation with an oral VKA (Grade 1A).[5]
- CCS Recommendations
- Oral anticoagulants are recommended for all AF patients aged 65 or older or who have any one of the traditional CHADS2 risk factors of stroke, hypertension, heart failure, or diabetes (remember as CHADS-65). Otherwise, patients with a history of coronary artery disease or arterial vascular disease should be prescribed ASA. CCS recommends that the first choice for oral anticoagulation should be the novel direct-acting oral anticoagulants (i.e. NOACs, for non-valvular AF). The big paradigm change is that ED physicians should prescribe OACs to at-risk AF patients before they leave the ED.[6]
CHADS2-VAsc Score
| Risk Factor | Points | ||||
| CHF | 1 | ||||
| hypertension | 1 | ||||
| DM | 1 | ||||
| Previous stroke/TIA | 2 | ||||
| Vascular disease (e.g. IHD, PVD) | 1 | ||||
| Female sex | 1 | ||||
| Age | |||||
|---|---|---|---|---|---|
| ≥ 75 years old | 2 | ||||
| 65 to 74 years old | 1 | ||||
- Score 0: consider no treatment or ASA
- Score 1: consider warfarin or ASA
- Score 2-6: consider warfarin (INR goal = 2-3)
- All patients with significant valvular disease should be on anticoagulation
HAS-BLED[7]
Used to assess 1 yr risk of bleeding on OAC medications
| Risk Factor | Point |
| Hypertension | 1 |
| Abnormal renal and/or hepatic function | 1 point each |
| Stroke | 1 |
| Bleeding tendency/predisposition | 1 |
| Labile INR on warfarin | 1 |
| Elderly (age >65 years) | 1 |
| Drugs (aspirin or NSAIDs) and/or alcohol | 1 point each |
- Score 1: 1.0 bleeds per 100 patient-years
- Score 2: 1.9 bleeds per 100 patient-years
- Score 3: 3.7 bleeds per 100 patient-years
- Score 4: 8.7 bleeds per 100 patient-years
- Score 5-9: Insufficient Data
Disposition
Similar outcomes for Canadian vs. American strategies, despite lower admission rates in Canada[8]
Canadian
- "Limit hospital admission to highly symptomatic patients in whom adequate rate control cannot be achieved"[9]
American
Indications for hospitalization:
- Patient with acute heart failure or hypotension after rhythm or rate control
- AF secondary to hypertension, infection, COPD exacerbation, PE, ACS/MI
- Age > 60 (high risk of thromboembolism, more likely to have comorbidities)
- Initiation of heparin or other anticoagulant
- If considering ablation of accessory pathway in patient with AF
- Symptomatic recurrence in the ED
- Hemodynamic instability
Indications for discharge (low-risk patients): Discharge with urgent cardiology follow up
- <60 years old
- No significant comorbid disease
- No clinical suspicion for PE or MI
- Conversion in ED or rate control
Complications
- Hemodynamic compromise
- A-fib lowers CO by 20-30%
- Impaired coronary blood flow
- Arrhythmogenesis
- Arterial thromboembolism
See Also
References
- ↑ 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: Executive Summary. J Am Coll Cardiol. 2014;64(21):2246-2280. doi:10.1016/j.jacc.2014.03.021
- ↑ 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: Executive Summary. J Am Coll Cardiol. 2014;64(21):2246-2280. doi:10.1016/j.jacc.2014.03.021
- ↑ Atrial Fibrillation: Would You Prefer a Pill or 150 Joules? Ann Emerg Med. 2015;66:655-657.
- ↑ EBQ:48hr Cardioversion for Afib]]
- ↑ 5.0 5.1 Singer DE et al. Antithrombotic therapy in atrial fibrillation: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition).Chest. 2008 Jun;133(6 Suppl):546S-592S
- ↑ Verma A, et al. 2014 Focused Update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation Canadian Journal of Cardiology 30 (2014) 1114e1130
- ↑ Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 2010; 138:1093.
- ↑ Rising KL. Home is Where the Heart Is. Annals of Emergency Medicine. 2013;62(6):578-579
- ↑ Stiell, et al. Atrial Fibrilation Guidelines. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: management of recent-onset atrial fibrilation and flutter in the emergency department. Can J Cardiolol. 2011;27:38-46