We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Lyme disease
From WikEM
(Redirected from Borrelia burgdorferi)
Contents
Background
- Tick Borne - Ixodes black-legged ticks
- Endemic Areas: NE, E US Coasts
- Caused by spirochete Borrelia burgdorferi
- The spirochete Borrelia mayonii has been a new strain implicated in cases in the midwest[1]
- Peak in May to Aug
- Stages: Early localized infection, early disseminated, and late disseminated
Clinical Features

"Classic" bull's-eye rash (i.e. erythema migrans) found in 70%-80% of cases[2]
3 Distinct Stages - Not all patients suffer all stages, and stages may overlap with remissions between stages
Early Localized Infection (7-14d)
- Erythema Chronicum Migrans: Occurs at site of tick bite, beginning with red macule that expands outward. Starts 3-30 days after bite and occurs in 70-80% of cases
- Erythema migrans rash more often without central clearing
- Fatigue, low grade fever, migrating arthralgia, lymphadenopathy, headache, nausea/vomiting, abdominal pain
Early Disseminated Infection (Days to weeks)
- Skin-mult annular lesions sparing palm/soles
- Nervous System-fluctuating meningoencephalitis, headache, nausea/vomiting, cranial nerve palsies (ie 7th-can be bilateral) peripheral neuropathy, radiculopathy
- Cardiovascular: AV blocks, RBBB, dysrhythmias, LV dysfunction
- Eye: Conjunctivitis, keratitis, retinal detachment, optic neuritis
Late Disseminated Infection (Months to Years)
- Arthritis: Monarticularule outligoarticular asymmetric arthritis (large joints-commonly knee)
- Brief episodes separated with complete remission
- Migratory pattern may occur
- Nervous System: Subtle encephalopathy, fatigue, polyneuropathy
Differential Diagnosis
- Enterovirus
- Hepatitis
- Mononucleosis
- Connective tissue disease
- Erythema Multiforme
- CAD
- Acute rheumatic fever
- Aseptic Meningitis
- HSV encephalitis
- Bell's Palsy
- Multiple Sclerosis
- Guillain-Barre
- Cerebral vasculitis
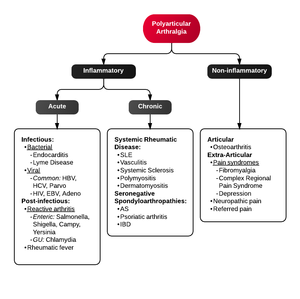
Polyarthritis
- Fibromyalgia
- Juvenile idiopathic arthritis
- Lyme disease
- Osteoarthritis
- Psoriatic arthritis
- Reactive poststreptococcal arthritis
- Rheumatoid arthritis
- Rheumatic fever
- Serum sickness
- Systemic lupus erythematosus
- Serum sickness–like reactions
- Viral arthritis
Tick Borne Illnesses
- Babesiosis
- Ehrlichiosis
- Lyme
- Rocky mountain spotted fever
- Tularemia
- STARI
- Heartland virus
- Tick paralysis
- Murine typhus
Evaluation
- ELISA if positive obtain confirmatory Western blot
- PCR
- Cultures, serologies
- LP with lymphocytic pleocytosis, elevated protein, normal glucose, + spirochete antibody, paired serum/CSF serologic tests,PCR
- Must be performed in patients with neuro findings (facial nerve palsy, meningoencephalitis, etc)
- CNS Lyme disease will be treated with ceftriaxone
- Arthrocentesis, serologic testing of fluid
Management
No risk when duration of attachment <24 hrs
Prophylaxis
- Adult: Doxycycline 200mg PO x1
- Child >8: 4mg/kg up to 200mg PO x1
- Give if all of the following are met:
- Tick is adult/nymphal I. scapularis
- Tick was attached >36 hours based on degree of engorgement or exposure time
- Prophylaxis can be given within 72 hrs after time tick was removed
- Local rate of infection in ticks >20%
- Doxycycline is not contraindicated
- Old vaccine has little to no efficacy after 1 year
Early Localized Infection
- Treat before serologic testing if endemic area if + erythema migrans rash
- Doxycycline 100mg PO BID x 14-21 days[3]
- Also treats human granulocytic ehrlichiosis
- Amoxicillin 500mg PO TID x 14-21 days
- Preferred in pregnant, lactating, children <8
- Cefuroxime axetil 500mg PO BID x 14-21 days
- Macrolides-not first line
- Doxycycline 100mg PO BID x 14-21 days[3]
- Jarisch-Herxheimer like reaction can occur in first 24 hrs of treatment (fevers, chills, myalgia, tachycardia)
Early Disemminated
- Doxycycline (see above dosing)
- Amoxicillin (See above dosing)
Lyme Meningitis
- Ceftriaxone 2g IVq12h x 14-28 days
- Doxycycline 200-400mg/d divided into two doses q day x 10-28 days
- Penicillin G, Cefotaxime
Cardiac Disease
- Mild (1st degree AV with PR <0.3 sec)
- Severe (HIgh-degree AV block)
- Ceftriaxone/Pen G IV
Arthritis
- Doxycycline, Amoxicillin PO, as effective as parenteral
- Ceftriaxone/Pen G IV
Disposition
Outpatient
- Early Disease
- Late Disease: If chronic neurologic/arthritic manifestations may be able to manage as outpatient
- Follow up with primary care, rheum, ID
Admission
- Lyme carditis-cardiac monitoring
- Prominent neurologic symptoms for IV antibiotics and further care
See Also
References
- ↑ Pritt BS, Mead PS, Johnson DKH, et al.Identification of a novel pathogenic Borrelia species causing Lyme borreliosis with unusually high spirochaetaemia: a descriptive study. Lancet Infectious Disease. Published Online: 05 February 2016.
- ↑ Signs and Symptoms of Lyme Disease, CDC, page last reviewed: June 16, 2015.
- ↑ Shapiro, E. (2014) ‘Lyme disease’, New England Journal of Medicine, 371(7), pp. 683–684.