We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Cerebral venous thrombosis
From WikEM
The cavernous sinus is one of the several cerebral veins and cavernous sinus thrombosis is a specific type of cerebral venous (sinus) thrombosis. See that article for a discussion of that specific clinical entity.
Contents
Background
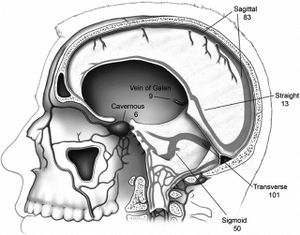
- Occlusion of venous sinus (most commonly superior sagittal and lateral sinuses) by thrombus[1]
- No precise prevalence or incidence established due to rarity of condition. However the disease is more prevalent in patients with thrombilia, oral contraceptive use, and during pregnancy.[2]
- Median Age ~ 37 years[2]
- Female:Male ratio 3:1[2]
Predisposing factors
- Cancer
- Pregnancy
- Local infections (otitis media, sinusitis, cellulitis)
- Hypercoagulable states
- Trauma
- Drugs (ecstasy, androgens, OCPs)
- Compression of venous sinus (tumor, abscess)
Clinical Features
Clinical presentation varies depending on location, acuity, and severity of thrombosis. More gradual onset of symptoms or thrombosis allows for compensatory collateral venous system to develop
Common Symptoms
Symptoms are variable and may not all be present[3]
- Headache 74-92%
- Seizures 35-50%
- Papilledema 28-45%
- Focal Neurologic sequelae (seizures, dizziness) 25-71%
- Encephalopathy
Neurodefecits
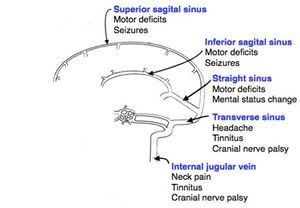
Although presentation can be highly variable, neurodefecits can be correlated with the location of the occlusion[3]
- Superior Sagital sinus - motor deficits, seizures
- Left transverse sinus - aphasia
- Cavernous sinus - ocular pain, protosis, oculomotor palsies
- Deep venous sinus -thalamic related symptoms such as altered mental status
Differential Diagnosis
Headache
Common
Killers
- Meningitis/encephalitis
- Retropharyngeal abscess
- Intracranial Hemorrhage (ICH)
- SAH / sentinel bleed
- Acute obstructive hydrocephalus
- Space occupying lesions
- CVA
- Carbon monoxide poisoning
- Basilar artery dissection
- Preeclampsia
- Cerebral venous thrombosis
- Hypertensive emergency
- Depression
Maimers
- Temporal arteritis
- Idiopathic intracranial hypertension (aka Pseudotumor Cerebri)
- Acute Glaucoma
- Acute sinusitis
- Cavernous sinus thrombosis or cerebral sinus thrombosis
Others
- Trigeminal neuralgia
- TMJ pain
- Post-lumbar puncture headache
- Dehydration
- Analgesia abuse
- Various ocular and dental problems
- Herpes zoster ophthalmicus
- Herpes zoster oticus
- Cryptococcosis
- Febrile headache (e.g. pyelonephritis, nonspecific viral infection)
- Ophthalmoplegic migraine
- Superior Vena Cava Syndrome
Aseptic Meningitis
- Viral
- Varicella
- Herpes
- Enterovirus
- West Nile
- Tuberculosis
- Lyme disease
- Syphilis
- Drug induced aseptic meningitis
- Fungal (AIDS, transplant, chemotherapy, chronic steroid use)
- Noninfectious
- Sarcoidosis
- Vasculitis
- Connective tissues disease
Evaluation
Suspect in patients with headache, signs of increased ICP, or focal neurologic deficits, especially if any of above predisposing factors are present
Imaging
- MRI and MRV are considered diagnostic study of choice[4]
- CT venography is a reasonable alternative if there is a contraindication to MRV and may have a similar sensitivity to MRV in recent studies[4]
- May see "Empty delta sign" dense triangle in superior sagittal sinus[5]
- Cord sign: thrombus in the cerebral sinus may appear as a hyperattenuated foci. It is homogenous in nature and appears linear or round based on the affected sinus. This is most commonly seen in the first week. [6]
- Vein Sign: After two weeks, the thrombus becomes hypoattenuated. When the thrombus is located in the deep vein it is referred to as the vein sign. [7]
- Non contrast CT possesses insufficient sensitivity or specificity to be of diagnostic value in the setting of high clinical suspicion
Labs
- D-Dimer is not a reliable test to rule out a cerebral venous thrombosis[8]
- In patients with a concern for meningitis then pursue diagnosis via standard workup which includes a CT before lumbar puncture
Management
Anticoagulation
- Heparin or low molecular weight heparin
- Of note, heparin initial bolus is 3000-5000U, lower than the dosing for PE/DVT
- Eventual transition to oral anticoagulation for a 3-6 month duration
Seizure prophylaxis
Supportive care
- Frequent neurologic checks and clinical monitoring for increased ICP
- Neurology or neurosurgical consultation depending on institutional resources
Acute Decompensation
- If persistent or severe elevated intracranial pressure a hemicraniectomy may be necessary
- Intravascular thrombolytics (either catheter guided or systemic) in coordination with neurology may be required if the patient experiences rapidly progressing decompensation[10]
Disposition
- Admission
- To a level of care capable of frequent neurologic monitoring. Inpatient, the patient should also have a evaluation for a coagulopathy.
See Also
References
- ↑ Piazza G. Cerebral venous thrombosis. Circulation 2012;125:1704-1709.
- ↑ 2.0 2.1 2.2 Bousser MG, Ferro JM. Cerebral venous thrombosis: an update. Lancet Neurol 2007; 6:162-70.
- ↑ 3.0 3.1 Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med 2005;352:1791–8.
- ↑ 4.0 4.1 Khandelwal N et al. Comparison of CT venography with MR venography in cerebral sinovenous thrombosis. AJR Am J Roentgenol 2006;187:1637–1643.
- ↑ Lee Emil J. Y. “The Empty Delta Sign.” Radiology. 224(3). 2002. 788-789.
- ↑ Ram K. P. Vijay. "The Cord Sign."Radiology. 2006; 240:299-300.
- ↑ Linn J, Pfefferkorn T. "Noncontrast CT in Deep Cerebral Venous Thrombosis and Sinus Thrombosis: Comparison of Its Diagnostic Value for Both Entities."AJNR Am J Neuroradiology. 2010; 30: 728-735.
- ↑ Crassard I, Soria C, Tzourio C, Woimant F, Drouet L, Ducros A, Bousser MG. A negative D-dimer assay does not rule out cerebral venous thrombosis: a series of seventy-three patients. Stroke 2005;36:1716 –1719.
- ↑ Ferro JM et al. Early seizures in cerebral vein and dural sinus thrombosis: risk factors and role of antiepileptics. Stroke 2008;39:1152–1158.
- ↑ 38.Dentali F et al. Safety of thrombolysis in cerebral venous thrombosis: a systematic review of the literature. Thromb Haemost 2010;104:1055–1062.