We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Acute coronary syndrome (main)
From WikEM
(Redirected from Myocardial infarct)
For risk stratification see ACS - Risk Stratification
Contents
Background
- Abbreviation: ACS
- Refers to a spectrum of conditions compatible with acute myocardial ischemia and/or infarction that are usually due to an abrupt reduction in coronary blood flow.
- ST-Elevation Myocardial Infarction (STEMI) (30%)
- Non ST-Elevation Myocardial Infarction (NSTEMI) (25%),
- Unstable Angina (38%)
- The new title, “Non-ST-Elevation Acute Coronary Syndromes,” emphasizes the continuum between UA and NSTEMI[1]
- NSTEMI myocardium is damaged enough to increase biomarkers, UA is not.
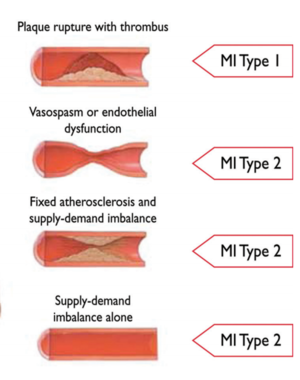
MI Types by Causation[2]
- Type 1 - Spontaneous Myocardial Infarction
- Atherosclerotic plaque rupture or intraluminal thrombus in one or more of the coronary arteries
- Type 2 - Myocardial Infarction Secondary to an Ischaemic Imbalance
- Condition other than CAD contributes to an imbalance between myocardial oxygen supply and/or demand
- Type 3 - Cardiac Death Due to Myocardial Infarction
- Suffer cardiac death with symptoms suggestive of myocardial ischaemia without elevated biomarkers
- Type 4 - Myocardial Infarction Associated With Revascularization Procedure
- 4a: Related to PCI
- 4b: Related to Stent Thrombosis
- Type 5 - Myocardial Infarction Related to CABG Procedure
Prognosis
Clinical Features
Risk of ACS
Clinical factors that increase likelihood of ACS/AMI:[3][4]
- Chest pain radiating both arms >R arm >L arm
- Chest pain associated with diaphoresis
- Chest pain associated with nausea/vomiting
- Chest pain with exertion
Clinical factors that decrease likelihood of ACS/AMI:[5]
- Pleuritic chest pain
- Positional chest pain
- Sharp, stabbing chest pain
- Chest pain reproducible with palpation
Male and female patients typical present with similar symptoms[6]
Differential Diagnosis
Chest pain
Critical
- Acute Coronary Syndromes
- Aortic Dissection
- Cardiac Tamponade
- Pulmonary Embolism
- Tension Pneumothorax
- Boerhhaave's Syndrome
- Coronary Artery Dissection
Emergent
- Pericarditis
- Myocarditis
- Pneumothorax
- Mediastinitis
- Cholecystitis
- Pancreatitis
- Cocaine-associated chest pain
Nonemergent
- Stable angina
- Asthma exacerbation
- Valvular Heart Disease
- Aortic Stenosis
- Mitral valve prolapse
- Hypertrophic cardiomyopathy
- Pneumonia
- Pleuritis
- Tumor
- Pneumomediastinum
- Esophageal Spasm
- Gastroesophageal Reflux Disease (GERD)
- Peptic Ulcer Disease
- Biliary Colic
- Muscle sprain
- Rib Fracture
- Arthritis
- Chostochondirits
- Spinal Root Compression
- Thoracic outlet syndrome
- Herpes Zoster / Postherpetic Neuralgia
- Psychologic / Somatic Chest Pain
- Hyperventilation
- Panic attack
Elevated Troponin
True Positive
False (Non-CAD) Positives
- Pericarditis
- PE
- CHF
- Sepsis
- Dissection
- Arrhythmias
- CVA
- SAH
- Burns
- Renal failure
- Assume true positive until proven otherwise
- Cardioversion
- Cardiotoxic medications
- Amyloidosis
- Rheumatoid Factor
- Heterophilic antibodies
Evaluation
Workup
- ECG (Diagnosis)
- ECG is normal in 8% of all confirmed MI's
- In LBBB see Sgarbossa's Criteria
- Cardiac Enzymes
Evaluation
ACS Anatomical Correlation Chart
| Ischemic Changes | Location | Coronary Artery |
| STE V1-V3, TWI Q waves in V1-V3 over time |
Septal | Septal branch |
| STE V2-V4 | Anterior | LAD |
| STE I, aVL, V5, V6 STD inf leads |
Lateral | Circumflex |
| STE I, aVL, V2-6 | Anterolateral | LAD + circumflex = Left main or 2 critical lesions |
| STE II, III, aVF STD in aVL (most common lead to see reciprocal change) |
Inferior | RCA |
|
STE V1 (only lead looking at RV)
|
Right ventricle | RCA |
|
STD in V1, V2, V3; |
Posterior aka Inferolateral | RCA (90%), LCA (10%) |
| STE avR>V1 Doesn't apply in SVT |
Anterolateral | Left Main |
Management
Intensity of treatment should be based on ACS likelihood
- ST-Elevation Myocardial Infarction (STEMI)
- Non ST-Elevation Myocardial Infarction (NSTEMI)
- Unstable Angina
Disposition
- Admit
- Ischemic ECG changes
- Pacemakers
- LBBB
- Positive troponins
- Abnormal vital signs
- ACC/AHA rec need for provocative testing withing 72 hrs, consider admitting
- For low risk (HEART) pts, may be better off discharge home with follow up[7]
- Risk of MACE after neg ED work up 1/2422 vs Risk of preventable adverse event in hospital is 1/164
External Links
- MDCalc - Framingham Coronary Heart Disease Risk Score
- MDCalc - Sgarbossa’s Criteria for MI in Left Bundle Branch Block
- MDCalc - TIMI Risk Score for UA/NSTEMI
- Heart Association
See Also
- ACS - Risk Stratification
- ACS - Anatomical Correlation
- ACS - Stress Testing
- ST-Elevation Myocardial Infarction (STEMI)
- NSTEMI
- Unstable Angina
- Unstable Angina - NSTEMI Guidelines
- Cocaine Chest Pain
- STEMI equivalents
References
- ↑ AHA ACA - NSTEMI ACS Guidelines 2014 View Online
- ↑ Third Universal Definition of Myocardial Infarction http://circ.ahajournals.org/content/126/16/2020.full.pdf
- ↑ Body R, Carley S, Wibberley C, et al. The value of symptoms and signs in the emergent diagnosis of acute coronary syndromes. Resuscitation. 2010;81(3):281–286. PMID: 20036454
- ↑ Panju AA, Hemmelgarn BR, Guyatt GH, et al. The rational clinical examination. Is this patient having a myocardial infarction? JAMA. 1998;280(14):1256–1263. PMID: 9786377
- ↑ Swap CJ, Nagurney JT. Value and limitations of chest pain history in the evaluation of patients with suspected acute coronary syndromes. JAMA. 2005;294(20):2623–2629. PMID: 16304077
- ↑ Gimenez MR, et al. Sex-specific chest pain characteristics in the early diagnosis of acute myocardial infarction. JAMA Intern Med. 2014; 174(2):241-249.
- ↑ Weinstock MB, Weingart S, Orth F, VanFossen D, Kaide C, Anderson J, Newman DH. Risk for Clinically Relevant Adverse Cardiac Events in Patients With Chest Pain at Hospital Admission. JAMA Intern Med. 2015 Jul;175(7):1207-12.