We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Pulmonary edema
From WikEM
(Redirected from Pulmonary Edema)
Contents
Background
Pulmonary Edema Types
Cardiogenic pulmonary edema
Noncardiogenic pulmonary edema
- Negative pressure pulmonary edema
- Upper airway obstruction
- Reexpansion edema
- Neurogenic causes
- Iatrogenic fluid overload
- Multiple blood transfusions
- IV fluid
- Inhalation injury
- Pulmonary contusion
- Aspiration pneumonia and pneumonitis
- Other
Clinical Features
- Crackles
- Respiratory distress
- Increased jugular venous distension
- Signs of poor organ perfusion
Differential Diagnosis
Shortness of breath
Emergent
- Pulmonary
- Airway obstruction
- Anaphylaxis
- Aspiration
- Asthma
- Cor pulmonale
- Inhalation exposure
- Noncardiogenic pulmonary edema
- Pneumonia
- Pneumocystis Pneumonia (PCP)
- Pulmonary embolism
- Pulmonary hypertension
- Tension pneumothorax
- Idiopathic pulmonary fibrosis acute exacerbation
- Cardiac
- Other Associated with Normal/↑ Respiratory Effort
- Other Associated with ↓ Respiratory Effort
Non-Emergent
- ALS
- Ascites
- Uncorrected ASD
- Congenital heart disease
- COPD exacerbation
- Fever
- Hyperventilation
- Neoplasm
- Obesity
- Panic attack
- Pleural effusion
- Polymyositis
- Porphyria
- Pregnancy
- Rib fracture
- Spontaneous pneumothorax
- Thyroid Disease
Evaluation
- CBC (rule out anemia)
- Chem
- ECG
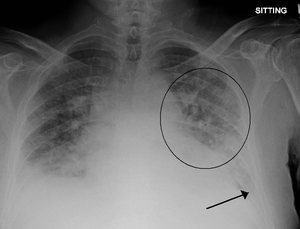
- CXR
- Cephalization
- Interstitial edema
- Pulmonary venous congestion
- Pleural effusion
- Alveolar edema
- Cardiomegaly
- Troponin?
- Ultrasound
- Bedside to assess global function, B lines, assessment of IVC
- Formal TTE/TEE
Brain natriuretic peptide (BNP)[1]
- Biologically active metabolite of proBNP (released from ventricles in response to increased volume/pressure)
- Utility is controversial and may not affect patient centered outcomes[2]
- May be trended to gauge treatment response in acute decompensated CHF
- May have false negative with isolated diastolic dysfunction
- Measurement
- <100 pg/mL: Negative for acute CHF (Sn 90%, NPV 89%)
- 100-500 pg/mL: Indeterminate (Consider differential diagnosis and pre-test probability)
- >500 pg/mL: Positive for acute CHF (Sp 87%, PPV 90%)
NT-proBNP[3][4][5]
- N-terminal proBNP (biologically inert metabolite of proBNP)
- <300 pg/mL → CHF unlikely
- CHF likely in:
- >450 pg/mL in age < 50 years old
- >900 pg/mL in 50-75 years old
- >1800 pg/mL in > 75 years old
Differential Diagnosis (Elevated BNP)
BNP In Obese Patients
- Visceral fat expansion leads to increased clearance of active natriuretic peptides[6]
- Obese patients also frequently treated for hypertension or coronary artery disease which may also contribute to lower BNP levels
Interpretation
- In one study of 204 patients with acute CHF, an inverse relationship between BMI and BNP was noted. The standard cutoff of 100pg/mL resulted in a 20% false-negative rate[7]
- Analysis of a subgroup of patients with documented BMI from the Breathing Not Properly study showed that a lower cutoff was more appropriate to maintain 90% sensitivity in obese and morbidly obese patients (54pg/mL)[8]
Management
- CPAP/BiPAP with PEEP 6-8; titrate up to PEEP of 10-12
- Nitroglycerin
- Dosing Options
- Sublingual 0.4mg q5min
- Nitropaste (better bioavailability than oral Nitroglycerin)
- Intravenous: 0.1mcg/kg/min - 5mcg/kg/min
- Generally start IV Nitroglycerin 50mcg/min and titrate rapidly (150mcg/min or higher) to symptom relief
- Nursing may be resistant. Explain that 1 SL tab (400 mcg) Q4min = 100 mcg/min for perspective.
- Dosing Options
- If NTG fails to reduce BP consider nitroprusside (reduces both preload and afterload) or ACE-inhibitiors (preload reducer)
- After patient improves titrate down NTG as enaliprilat (0.625 - 1.25mg IV) or captopril are started
- Morphine is no longer recommended do to increased morbidity[9][10]
Disposition
See Also
- Congestive Heart Failure (CHF)
- Acute Respiratory Distress Syndrome
- Sympathetic crashing acute pulmonary edema (SCAPE)
References
- ↑ Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347(3):161-167. doi:10.1056/NEJMoa020233.
- ↑ Carpenter CR et al. BRAIN NATRIURETIC PEPTIDE IN THE EVALUATION OF EMERGENCY DEPARTMENT DYSPNEA: IS THERE A ROLE? J Emerg Med. 2012 Feb; 42(2): 197–205.
- ↑ Januzzi JL, van Kimmenade R, Lainchbury J, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study. Eur Heart J. 2006 Feb. 27(3):330-7.
- ↑ Kragelund C, Gronning B, Kober L, Hildebrandt P, Steffensen R. N-terminal pro-B-type natriuretic peptide and long-term mortality in stable coronary heart disease. N Engl J Med. 2005 Feb 17. 352(7):666-75.
- ↑ Moe GW, Howlett J, Januzzi JL, Zowall H,. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation. 2007 Jun 19. 115(24):3103-10.
- ↑ Clerico A, Giannoni A, Vittorini S, Emdin M. The paradox of low BNP levels in obesity. Heart Fail Rev. 2011;17(1):81-96. doi:10.1007/s10741-011-9249-z.
- ↑ Krauser DG, Lloyd-Jones DM, Chae CU, et al. Effect of body mass index on natriuretic peptide levels in patients with acute congestive heart failure: A ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE) substudy. Am Heart J. 2005;149(4):744-750. doi:10.1016/j.ahj.2004.07.010.
- ↑ Daniels LB, Clopton P, Bhalla V, et al. How obesity affects the cut-points for B-type natriuretic peptide in the diagnosis of acute heart failure. Results from the Breathing Not Properly Multinational Study. Am Heart J. 2006;151(5):999-1005. doi:10.1016/j.ahj.2005.10.011.
- ↑ Peacock WF, Hollander JE, Diercks DB, Lopatin M, Fonarow G, Emerman CL. Morphine and outcomes in acute decompensated heart failure: an ADHERE analysis. Emerg Med J. 2008 Apr;25(4):205-9.
- ↑ Ellingsrud C, Agewall S. Morphine in the treatment of acute pulmonary oedema--Why? Int J Cardiol. 2016 Jan 1;202:870-3.