We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Supracondylar fracture
From WikEM
Contents
Background
- Most common elbow fracture in patients age <8yr
- 95% are extension type (FOOSH mechanism)
Clinical Features
Do not encourage active/passive elbow movement until displaced fracture has been ruled-out
- Pain, swelling, very limited range of motion
- Non-displaced fracture may have limited swelling, but child will refuse to move arm
- TTP of posterior, distal humerus
- If evidence of S-shape configuration or skin dimpling, splint before xray
Differential Diagnosis
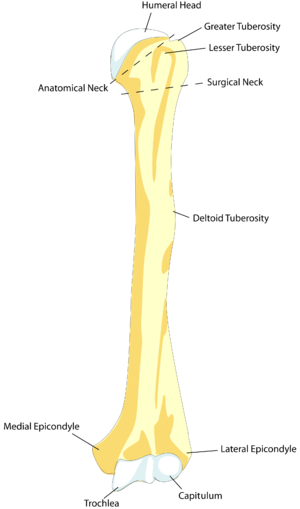
Humerus Fractures
Elbow Diagnoses
Radiograph-Positive
Radiograph-Negative
- Lateral epicondylitis
- Medial epicondylitis
- Olecranon bursitis (nonseptic)
- Septic bursitis
- Biceps tendon rupture/dislocation
Pediatric
- Nursemaid's elbow
- Supracondylar fracture
- Lateral epicondyle fracture
- Medial epicondyle fracture
- Olecranon fracture
- Radial head fracture
- Salter-Harris fractures
Evaluation
Imaging
- True lateral elbow
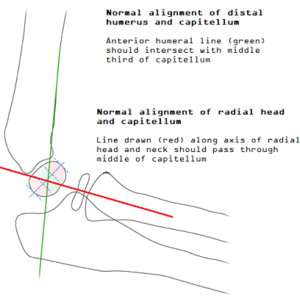
- Anterior humeral line should intersect with middle third of capitellum (see pediatric elbow alignment)
- If not, consider supracondylar fracture (or lateral condyle fracture)
- Anterior humeral line should intersect with middle third of capitellum (see pediatric elbow alignment)
- Forearm/wrist views
- Co-injuries are common with elbow fracture
Gartland Classification
- Type I
- Nondisplaced with evidence of elbow effusion (ant sail sign and/or posterior fat pad)
- Type II
- Displaced with intact posterior periosteum
- Anterior humeral line is displaced anteriorly relative to capitellum
- Type III
- Displaced with disruption of anterior and posterior periosteum
- If distal fragment is posteromedially displaced: radial nerve injury
- If distal fragment is posterolaterally displaced: median nerve, brachial artery injury
- Displaced with disruption of anterior and posterior periosteum
Management & Disposition
- Type I
- Immobilize using double sugar tong or long-arm posterior splint x3wk
- Elbow at 90degrees, forearm in pronation or neutral rotation
- Refer to ortho within 48hr
- Immobilize using double sugar tong or long-arm posterior splint x3wk
- Types II & III
- Orthopedic consult in the ED
- Admit
Complications
Vascular
- Volkmann Ischemic Contracture (Compartment Syndrome of forearm)
- Occurs more commonly when forearm is also fractured
- Mere lack of a radial pulse does not indicate ischemia unless accompanied by:
- Refusal to open hand
- Pain with passive extension of fingers
- Forearm tendernes
- Brachial artery injury
- Suggested by ecchymosis over anteromedial aspect of forearm
- Strong collaterals might mask vascular injury
Neurologic
- Majority of nerve injuries are neuropraxias without long-term sequelae
- Median nerve injury
- Motor: Weakness of hand flexors (difficulty making "OK" sign), abduction of thumb
- Sensory: Altered two-point sensation on palmar surface of thumb, IF, MF
- Radial nerve injury
- Motor: Weakness of wrist extension, thumb extension (thumbs up)
- Sensory: Altered sensation in dorsal thumb-index web space
- Ulnar nerve injury
- Motor: Weakness of index finger abduction
- Sensory: Altered two-point discrimination over tip of little finger