Prevention
Today, more tools than ever are available to prevent HIV. In addition to abstinence, limiting your number of sexual partners, never sharing needles, and using condoms the right way every time you have sex, you may be able to take advantage of newer medicines such as pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP).
If you are living with HIV, there are many actions you can take to prevent passing it to others. The most important is taking medicines to treat HIV (called antiretroviral therapy, or ART) the right way, every day. They can keep you healthy for many years and greatly reduce your chance of transmitting HIV to your partners.
Is abstinence the only 100% effective HIV prevention option?
Yes. Abstinence means not having oral, vaginal, or anal sex. An abstinent person is someone who’s never had sex or someone who’s had sex but has decided not to continue having sex for some period of time. Abstinence is the only 100% effective way to prevent HIV, other sexually transmitted diseases (STDs), and pregnancy. The longer you wait to start having oral, vaginal, or anal sex, the fewer sexual partners you are likely to have in your lifetime. Having fewer partners lowers your chances of having sex with someone who has HIV or another STD.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
How can I prevent getting HIV from anal or vaginal sex?
Use condoms the right way every time you have sex, take medicines to prevent or treat HIV if appropriate, choose less risky sexual behaviors, get tested for other sexually transmitted diseases (STDs), and limit your number of sex partners. The more of these actions you take, the safer you can be.
Specifically, you can:
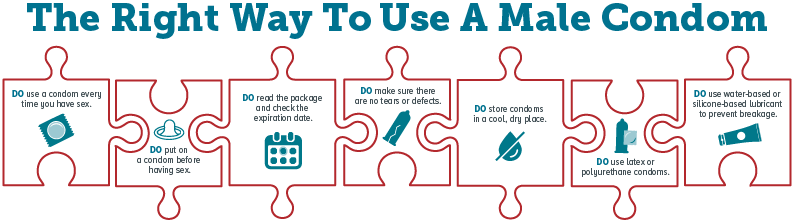
- Use condoms the right way every time you have sex (see How well do condoms prevent HIV?). Learn the right way to use a male condom.
- Reduce your number of sexual partners. This can lower your chances of having a sex partner who will transmit HIV to you. The more partners you have, the more likely you are to have a partner with HIV whose viral load is not suppressed or to have a sex partner with a sexually transmitted disease. Both of these factors can increase the risk of HIV transmission.
- Talk to your doctor about pre-exposure prophylaxis (PrEP), taking HIV medicines daily to prevent HIV infection, if you are at very high risk for HIV. PrEP should be considered if you are HIV-negative and in an ongoing sexual relationship with an HIV-positive partner. PrEP also should be considered if you aren’t in a mutually monogamous relationship with a partner who recently tested HIV-negative, and you are a:
- gay or bisexual man who has had anal sex without a condom or been diagnosed with an STD in the past 6 months;
- man who has sex with both men and women; or
- heterosexual man or woman who does not regularly use condoms during sex with partners of unknown HIV status who are at very high risk of HIV infection (for example, people who inject drugs or women who have bisexual male partners).
- Post-exposure prophylaxis (PEP) means taking HIV medicines after being potentially exposed to HIV to prevent becoming infected. If you’re HIV-negative or don’t know your HIV status and think you have recently been exposed to HIV during sex (for example, if the condom breaks), talk to your health care provider or an emergency room doctor about PEP right away (within 3 days). The sooner you start PEP, the better; every hour counts. If you’re prescribed PEP, you’ll need to take it once or twice daily for 28 days. Keep in mind that your chance of getting HIV is lower if your HIV-positive partner is taking medicine to treat HIV infection (called antiretroviral therapy, or ART) the right way, every day and his or her viral load remains suppressed (see Can I get HIV from someone who is HIV-positive but has an undetectable viral load?).
- Get tested and treated for other STDs and encourage your partners to do the same. If you are sexually active, get tested at least once a year. Having other STDs increases your risk for getting or transmitting HIV. STDs can also have long-term health consequences. Find an STD testing site.
- If you’re HIV-negative and your partner is HIV-positive, encourage your partner to get and stay on treatment. If taken the right way, every day, the medicine to treat HIV (ART) reduces the amount of HIV (called “viral load”) in the blood and elsewhere in the body to very low levels. This is called “viral suppression.” Being virally suppressed is good for an HIV-positive person’s overall health and greatly reduces the chance of transmitting the virus to a partner.
- Choose less risky sexual behaviors. HIV is mainly spread by having anal or vaginal sex without a condom or without taking medicines to prevent or treat HIV.
Receptive anal sex is the riskiest type of sex for getting HIV. It’s possible for either partner—the partner inserting the penis in the anus (the top) or the partner receiving the penis (the bottom)—to get HIV, but it is much riskier for an HIV-negative partner to be the receptive partner. That’s because the lining of the rectum is thin and may allow HIV to enter the body during anal sex.
Vaginal sex also carries a risk for getting HIV, though it is less risky than receptive anal sex. Most women who get HIV get it from vaginal sex, but men can also get HIV from vaginal sex.
In general, there is little to no risk of getting or transmitting HIV from oral sex. Theoretically, transmission of HIV is possible if an HIV-positive man ejaculates in his partner’s mouth during oral sex. However, the risk is still very low, and much lower than with anal or vaginal sex. Factors that may increase the risk of transmitting HIV through oral sex are oral ulcers, bleeding gums, genital sores, and the presence of other STDs, which may or may not be visible. See How can I prevent getting HIV from oral sex?
Sexual activities that don’t involve contact with body fluids (semen, vaginal fluid, or blood) carry no risk of HIV transmission but may pose a risk for other STDs.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
How can I prevent getting HIV from oral sex?
In general, there is little to no risk of getting or transmitting HIV from oral sex. Theoretically, transmission of HIV is possible if an HIV-positive man ejaculates in his partner’s mouth during oral sex. However, the risk is still very low, and much lower than with anal or vaginal sex.
Oral sex involves putting the mouth on the penis (fellatio), vagina (cunnilingus), or anus (anilingus). There’s little to no risk of getting or transmitting HIV through oral sex. Factors that may increase the risk of transmitting HIV through oral sex are oral ulcers, bleeding gums, genital sores, and the presence of other sexually transmitted diseases (STDs), which may or may not be visible.
While there is little to no risk of getting HIV from oral sex, using a barrier (for example, a condom, dental dam, or cut-open nonlubricated condom) can further reduce your risk of getting or transmitting HIV and protect you and your partner from some other STDs, including gonorrhea of the throat and hepatitis.
The risk is also lower if the HIV-positive partner is taking medicine to treat HIV (called antiretroviral therapy or ART), or if the HIV-negative partner is taking medicine to prevent HIV (called pre-exposure prophylaxis or PrEP). Both PrEP and ART need to be taken the right way every time in order to work.
Because your mouth may come into contact with feces or other body fluids during oral sex, it is important that you talk to a health care provider about your chances of getting hepatitis A and B. If you’ve never had hepatitis A or B, there are vaccines to prevent them. Your provider can help you decide if vaccination is right for you.
For more information, see Oral Sex and HIV Risk.
How To Use A Dental Dam As A Barrier For Oral Sex
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
How well do condoms prevent HIV?
If you use them the right way every time you have sex, condoms are highly effective in preventing HIV infection. But it’s important to educate yourself about how to use them the right way.
Condoms can also help prevent other sexually transmitted diseases (STDs) you can get through body fluids, like gonorrhea and chlamydia. However, they provide less protection against STDs spread through skin-to-skin contact, like human papillomavirus or HPV (genital warts), genital herpes, and syphilis.
There are two main types of condoms: male and female.
Male Condoms
- A male condom is a thin layer of latex, polyurethane, polyisoprene, or natural membrane worn over the penis during sex. Male Condom Dos and Don’ts.
- Latex condoms provide the best protection against HIV. Polyurethane (plastic) or polyisoprene (synthetic rubber) condoms are good options for people with latex allergies, but plastic ones break more often than latex ones. Natural membrane (such as lambskin) condoms have small holes in them, so they don’t block HIV and other STDs.
- Use water- or silicone-based lubricants to lower the chances that a condom will break or slip during sex. Don’t use oil-based lubricants (for example, Vaseline, shortening, mineral oil, massage oils, body lotions, and cooking oil) with latex condoms because they can weaken the condom and cause it to break. Don’t use lubricants containing nonoxynol-9. It irritates the lining of the vagina and anus and increases the risk of getting HIV.
Female Condoms
- A female condom is a thin pouch made of a synthetic latex product called nitrile. It’s designed to be worn by a woman in her vagina during sex. Female Condom Dos and Don’ts.
- When worn in the vagina, female condoms are comparable to male condoms at preventing HIV, other STDs, and pregnancy. Some people use female condoms for anal sex. We don’t currently know how well female condoms prevent HIV and other STDs when used by men or women for anal sex. But we do know that HIV can’t travel through the nitrile barrier.
- It is safe to use any kind of lubricant with nitrile female condoms.
Even if you use condoms the right way every time you have sex, there’s still a chance of getting HIV. For some individuals at high risk of getting or transmitting HIV, adding other prevention methods, like taking medicines to prevent and treat HIV, can further reduce their risk (see How can I prevent getting HIV from anal or vaginal sex?).
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can using a lubricant help reduce my HIV risk?
Yes, because lubricants can help prevent condoms from breaking or slipping.
Water-based and silicon-based lubricants are safe to use with all condoms. Oil-based lubricants and products containing oil, such as hand lotion, Vaseline, or Crisco, should not be used with latex condoms because they can weaken the condom and cause it to break. It is safe to use any kind of lubricant with nitrile female condoms. But lubricants containing nonoxynol-9 should not be used because nonoxynol-9 irritates the lining of the vagina and anus and increases the risk of getting HIV.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can male circumcision prevent HIV?
Circumcised men are less likely than uncircumcised men to get HIV from HIV-positive female partners, but circumcision doesn’t decrease their risk as much as other prevention options. There is no evidence that male circumcision decreases a woman’s risk of getting HIV, and the evidence about the benefits of circumcision among gay and bisexual men is inconclusive.
Circumcised men should take other actions, like using condoms the right way every time they have sex or taking medicine to prevent or treat HIV, to further reduce their risk of getting HIV or to protect their partners.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can I take medicines to prevent getting HIV?
If you are at very high risk for HIV from sex or injecting drugs, taking HIV medicines daily, called pre-exposure prophylaxis (or PrEP), can greatly reduce your risk of HIV infection. You can combine additional strategies with PrEP to reduce your risk even further.
Federal guidelines recommend that PrEP be considered for people who are HIV-negative and at very high risk for HIV. This includes anyone who is in an ongoing sexual relationship with an HIV-positive partner. It also includes anyone who:
- Is not in a mutually monogamous* relationship with a partner who recently tested HIV-negative, and
- Is a
- gay or bisexual man who has had anal sex without a condom or been diagnosed with an STD in the past 6 months;
- man who has sex with both men and women; or
- heterosexual man or woman who does not regularly use condoms during sex with partners of unknown HIV status who are at substantial risk of HIV infection (for example, people who inject drugs or women who have bisexual male partners).
PrEP is also recommended for people who’ve injected drugs in the past 6 months and have shared needles or works or been in drug treatment in the past 6 months.
If you have a partner who is HIV-positive and are considering getting pregnant, talk to your doctor about PrEP. It may be an option to help protect you and your baby.
PrEP involves daily medication and regular visits to a health care provider.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool.
* Mutually monogamous means that you and your partner only have sex with each other and do not have sex outside the relationship.
Can I take medicines to prevent HIV after exposure?
Yes. Taking medicine after being potentially exposed to HIV, called post-exposure prophylaxis (or PEP), can keep you from becoming infected. But PEP must be started within 72 hours after a possible exposure.
If you think you’ve recently been exposed to HIV during sex (for example, if the condom breaks) or through sharing needles and works to prepare drugs (for example, cotton, cookers, water), talk to your health care provider or an emergency room doctor about PEP right away. The sooner you start PEP, the better; every hour counts. If you’re prescribed PEP, you’ll need to take it once or twice daily for 28 days.
Someone who is on PEP should continue to use condoms with sex partners and safe injection practices while taking PEP.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool.
Can I get vaccinated to prevent HIV?
No. There is currently no vaccine that will prevent HIV infection or treat those who have it.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can I use microbicides to prevent HIV?
No. Microbicides are gels, films, or suppositories that can kill or neutralize viruses and bacteria. Researchers are studying both vaginal and rectal microbicides to see if they can prevent sexual transmission of HIV, but none are currently available for use.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
If I am living with HIV, how can I prevent passing it to others?
There are many actions you can take to lower your risk of transmitting HIV to a partner. The more actions you take, the safer you can be.
- The most important thing you can do is to take medicines to treat HIV infection (called antiretroviral therapy, or ART) the right way, every day. These medicines reduce the amount of virus (viral load) in your blood and body fluids. They can keep you healthy for many years and greatly reduce your chance of transmitting HIV to your partners if you have a very low or undetectable viral load.
- If you’re taking medicines to treat HIV (ART), follow your health care provider’s advice. Visit your health care provider regularly and always take your medicines as directed.
- Use condoms the right way every time you have sex. Learn the right way to use a male condom.
- Choose less risky sexual behaviors. Anal sex is the highest-risk sexual activity for HIV transmission. If your partner is HIV-negative, it’s less risky if they’re the insertive partner (top) and you’re the receptive partner (bottom) during anal sex. Oral sex is much less risky than anal or vaginal sex. Sexual activities that don’t involve contact with body fluids (semen, vaginal fluid, or blood) carry no risk of HIV transmission.
- If you inject drugs, never share your needles or works with anyone.
- Talk to your partners about pre-exposure prophylaxis (PrEP), taking HIV medicines the right way, every day to prevent HIV infection. See Can I take medicines to prevent getting HIV?
- Talk to your partners about post-exposure prophylaxis (PEP) if you think they’ve recently had a possible exposure to HIV (for example, if they had anal or vaginal sex without a condom or if the condom broke during sex). Your partners should talk to a health care provider right away (within 72 hours) after a possible exposure. Starting PEP immediately and taking it daily for 28 days will reduce their chance of getting HIV.
- Get tested and treated for other STDs and encourage your partners to do the same. If you are sexually active, get tested at least once a year. STDs can have long-term health consequences. They can also increase the risk of getting or transmitting HIV. Find an STD testing site.
Also, encourage your partners who are HIV-negative to get tested for HIV so they are sure about their status and can take action to keep themselves healthy. See How soon after an exposure to HIV can an HIV test detect if I am infected? To find a testing site near them, call 1-800-CDC-INFO (232-4636), visit gettested.cdc.gov, or text their ZIP code to KNOW IT (566948). Or they can use a home testing kit.
Learn more about how to protect your partners, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
How can I prevent getting HIV from drug use?
Stopping injection and other drug use can lower your chances of getting or transmitting HIV a lot. If you keep injecting drugs, use only sterile needles and works. Never share needles or works.
You are at very high risk for getting HIV if you use a needle or works after someone with HIV has used them. Also, when people are high, they’re more likely to have risky sex, which increases the chance of getting or transmitting HIV.
The best way to reduce your risk of HIV is to stop using drugs. You may need help to stop or cut down using drugs, but many resources are available. Talk with a counselor, doctor, or other health care provider about substance abuse treatment. To find a treatment center near you, check out the locator tools on SAMHSA.gov or HIV.gov, or call 1-800-662-HELP (4357).
If you keep injecting drugs, here are some things you can do to lower your risk for getting HIV and other infections:
- Use only new, sterile needles and works each time you inject. Many communities have needle exchange programs where you can get new needles and works, and some pharmacies may sell needles without a prescription.
- Never share needles or works.
- Clean used needles with bleach only when you can’t get new ones. Bleaching a needle may reduce the risk of HIV but doesn’t eliminate it.
- Use sterile water to fix drugs.
- Clean your skin with a new alcohol swab before you inject.
- Be careful not to get someone else’s blood on your hands or your needle or works.
- Dispose of needles safely after one use. Use a sharps container, or keep used needles away from other people.
- Get tested for HIV at least once a year.
- Ask your doctor about taking daily medicine to prevent HIV (called pre-exposure prophylaxis or PrEP).
- Don’t have sex if you’re high. If you do have sex, use a condom the right way every time. Learn the right way to use a male condom.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
How can I prevent passing HIV to my baby?
If you have HIV, the most important thing you can do is to take medicines to treat HIV infection (called antiretroviral therapy or ART) the right way, every day.
If you’re pregnant, talk to your health care provider about getting tested for HIV and other ways to keep you and your child from getting HIV. Women in their third trimester should be tested again if they engage in behaviors that put them at risk for HIV.
If you are HIV-negative but you have an HIV-positive partner and are considering getting pregnant, talk to your doctor about taking pre-exposure prophylaxis (PrEP) to help keep you from getting HIV. Encourage your partner to take medicines to treat HIV (ART), which greatly reduces the chance that he will transmit HIV to you.
If you have HIV, take medicines to treat HIV (ART) the right way, every day. If you are treated for HIV early in your pregnancy, your risk of transmitting HIV to your baby can be 1% or less. After delivery, you can prevent transmitting HIV to your baby by avoiding breastfeeding, since breast milk contains HIV.
For more information, see CDC’s HIV Among Pregnant Women, Infants, and Children.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Content provided and maintained by the US Centers for Disease Control and Prevention (CDC). Please see our system usage guidelines and disclaimer.
- Page last reviewed: June 6, 2017
- Page last updated: June 6, 2017
- Content source: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention


 ShareCompartir
ShareCompartir