HIV Among Pregnant Women, Infants, and Children
Fast Facts
- Women who are pregnant or planning a pregnancy should get tested for HIV as early as possible.
- If treated early in her pregnancy, a woman’s risk of transmitting HIV to her baby can be reduced to 1% or less.
- For children living with HIV, starting treatment early can help them live longer, healthier lives.
 Perinatal HIV transmission, also known as mother-to-child transmission, can happen at any time during pregnancy, labor, delivery, and breastfeeding. CDC recommends that all women who are pregnant or planning to get pregnant take an HIV test as early as possible before and during every pregnancy. This is because the earlier HIV is diagnosed and treated, the more effective HIV medicines, called antiretroviral treatment (ART), will be at preventing transmission and improving the health outcomes of both mother and child.
Perinatal HIV transmission, also known as mother-to-child transmission, can happen at any time during pregnancy, labor, delivery, and breastfeeding. CDC recommends that all women who are pregnant or planning to get pregnant take an HIV test as early as possible before and during every pregnancy. This is because the earlier HIV is diagnosed and treated, the more effective HIV medicines, called antiretroviral treatment (ART), will be at preventing transmission and improving the health outcomes of both mother and child.
Advances in HIV research, prevention, and treatment have made it possible for many women living with HIV to give birth without transmitting the virus to their babies. The annual number of HIV infections through perinatal transmission have declined by more than 90% since the early 1990s. Today, if a woman takes HIV medicines as prescribed throughout pregnancy, labor and delivery, and provides HIV medicines to her baby for 4-6 weeks, the risk of transmitting HIV can be 1% or less. In some cases, a Cesarean delivery can also prevent HIV transmission. After delivery, a mother can prevent transmitting HIV to her baby by not breastfeeding and not pre-chewing her baby’s food. For babies living with HIV, starting treatment early is important because the disease can progress more rapidly in children than adults. Providing ART early can help children with perinatal HIV live longer, healthier lives.
It is important that all women who are pregnant or trying to get pregnant encourage their partners to also get tested for HIV. Women who are HIV-negative but have an HIV-positive partner should talk to their doctor about taking HIV medicines daily, called pre-exposure prophylaxis (PrEP), to protect themselves while trying to get pregnant, and to protect themselves and their baby during pregnancy and while breastfeeding.
The Numbers
HIV Infections and Prevented Cases of Perinatal HIV Transmission
- Approximately 8,500 women living with HIV give birth annually (based on an estimate from 2006, the most recent available).
- Between 1994 and 2010, an estimated 21,956 cases of perinatally acquired HIV infections were prevented.
Rates of Perinatally Acquired HIV Infections by Year of Birth and Mother’s Race/Ethnicity, 2009–2013
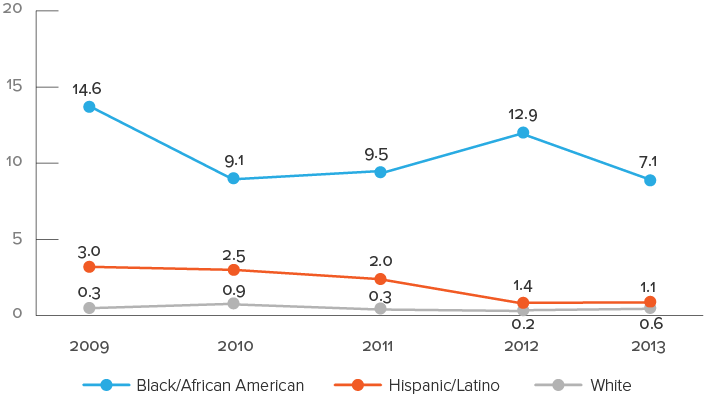
Data include only persons born in the United States.
Data accounted for delays between birth and diagnosis, as well as between diagnosis and reporting.
Rates are per 100,000 live births.
Live-birth data reflect race/ethnicity of the infant’s mother.
Hispanics/Latinos can be of any race.
Source: CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2014. HIV Surveillance Supplemental Report 2016;21(4).
Living With HIV
- Of the 1,995 childrena living with diagnosed perinatal HIV at the end of 2014, 1,288 (65%) were black/African American, 294 (15%) were Hispanic/Latinob, and 226 (11%) were white.
- At the end of 2014, 9,525 adults and adolescents (aged 13 and older) were living with HIV acquired through perinatal transmission. Of these, 60% (5,691) were black/African American, 23% (2,225) were Hispanic/Latino, and 12% (1,133) were white.
Deaths
- From the beginning of the epidemic through 2014, there were 5,419 deaths among people who acquired HIV through perinatal transmission and were ever diagnosed with AIDSc. Most of the deaths (82%) were among children (under age 13).
Prevention Challenges
- Pregnant women with HIV may not know they are infected. CDC recommends HIV testing for all women as part of routine prenatal care. According to CDC research, more women take the prenatal HIV test if the opt-out approach is used. Opt-out prenatal HIV testing means that a pregnant woman is told she will be given an HIV test as part of routine prenatal care unless she opts out, i.e., chooses not to have the test. In some parts of the country where HIV among women is more common, CDC recommends a second test during the third trimester of pregnancy. In 2016, the American Medical Association created a new Common Procedural Terminology (CPT) code that includes HIV testing in the Obstetric Panel allowing prenatal care providers to order just one panel inclusive of many standard serologic tests for pregnant women.
- Many HIV medical care providers don’t have the specialized expertise to address preconception care, family planning services, or prenatal care for women living with HIV. CDC and the François-Xavier Bagnoud Center (FXBC) lead the Expert Panel on Preconception Care and Reproductive Health for Persons Living with HIV. Its goal is to develop best practices and operational guidance for providing preconception care, family planning services, and prenatal care for women living with HIV.
-
Women living with HIV may not know they are pregnant, how to prevent or safely plan a pregnancy, or what they can do to reduce the risk of transmitting HIV to their baby. These women need to be advised to:
- Visit their health care provider regularly and take HIV medicines (antiretroviral treatment, or ART) as directed for their own health if they think they might want to become pregnant.
- When pregnant, take HIV medicines the right way every day throughout the pregnancy, labor, and delivery.
- After delivery, ensure their infants take HIV medicines.
- Avoid breastfeeding.
- Avoid pre-chewing food for an infant, toddler, or anyone else.
- The risk of perinatal HIV transmission is much higher if the mother’s antiretroviral HIV treatment is interrupted at any time during pregnancy, labor, or delivery, or if HIV medicines are not provided to her infant. Pregnant women living with HIV may have nausea during pregnancy that can interfere with taking medicines, and new mothers may not be able to see their HIV medical care provider consistently.
- Social and economic factors, especially poverty, affect access to all health care, and disproportionately affect people living with HIV. Pregnant women living with HIV may face more barriers to accessing medical care if they also use injection drugs, abuse other substances, or are homeless, incarcerated, mentally ill, or uninsured.
What CDC Is Doing
-
 CDC has developed a framework to guide federal agencies and other organizations in their efforts to reduce the rate of perinatal transmission of HIV to less than 1% among infants born to women with HIV and less than 1 perinatal transmission per 100,000 live births.
CDC has developed a framework to guide federal agencies and other organizations in their efforts to reduce the rate of perinatal transmission of HIV to less than 1% among infants born to women with HIV and less than 1 perinatal transmission per 100,000 live births. - CDC works with FXBC to lead the Elimination of Mother-to-Child HIV Transmission Stakeholders Group, a group of experts on maternal and child health, HIV and AIDS, policy, research, and surveillance. The Stakeholders Group develops action plans and distributes information to support the goal of eliminating perinatal transmission.
- CDC partnered with the American College of Obstetricians and Gynecologists, CityMatCH, the Pediatric AIDS Chicago Prevention Initiative, and the National Fetal and Infant Mortality Review Program to develop a model to help local health systems identify and address missed prevention and treatment opportunities for pregnant women living with HIV. CDC also funds the Fetal and Infant Mortality Review (FIMR)/HIV Prevention Methodology National Resource Center, which provides information and technical support to communities using, or interested in using, the methodology.
- CDC funds perinatal HIV prevention through Comprehensive HIV Prevention Programs for Health Departments. Key partner activities include promoting HIV testing and antiretroviral treatment for pregnant women and implementing the FIMR-HIV methodology.
a 13 years of age and younger
b Hispanics/Latinos can be of any race
c Includes deaths from any cause
Bibliography
- CDC. Diagnoses of HIV infection in the United States and dependent areas, 2015. HIV Surveillance Report 2016;27
- CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2014. HIV Supplemental Report 2016;21(4)
- Little KM, Taylor AW, Borkowf CB, et al. Perinatal Antiretroviral Exposure and Prevented Mother-to-child HIV Infections in the Era of Antiretroviral Prophylaxis in the United States, 1994-2010. Pediatr Infect Dis J 2017 Jan; 36(1), 66-71.
- Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. Recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States. AIDSinfo 2016; D1-D10. Accessed January 12, 2017.
- CDC. Pediatric HIV surveillance (through 2014). Slide set.
- Townsend CL, Cortina-Borja M, Peckham CS, de Ruiter A, Lyall H, Tookey, PA. Low rates of mother-to-child transmission of HIV following effective pregnancy interventions in the United Kingdom and Ireland, 2000–2006. AIDS 2008;22(8):973-81
- CDC. Achievements in public health: reduction in perinatal transmission of HIV infection—United States, 1985–2005. MMWR 2006;55(21):592-97.
- Fleming PL, Lindegren ML, Byers R, et al. Estimated number of perinatal HIV infections, U.S., 2000. Poster Exhibition: XIV International AIDS Conference. Barcelona, Italy. 2002 Jul 7–12;14: Abstract No. TuPeC4773.
- Whitmore SK, Zhang X, Taylor AW, Blair JM. Estimated number of infants born to HIV-infected women in the United States and five dependent areas, 2006. J Acquir Immune Defic Syndr 2011;57:218-22.
- Taylor AW, Little KM, Zhang X, et al. Estimated perinatal antiretroviral exposures, cases prevented and infected infants in the era of antiretroviral prophylaxis in the United States. 19th Conference on Retroviruses and Opportunistic Infections (CROI 2012). Seattle, WA. 2012 Mar 5-7; Abstract No. T-103: Poster 1000.
- Valverde E, Short W, Brady K, Frazier E, Beer L, Mattson C. HIV medical provider’s assessment of the reproductive plans of women receiving HIV care: Medical Monitoring Project Provider Survey, 2009. 6th IAS Conference on HIV Pathogenesis, Treatment and Prevention (IAS 2011). Rome, Italy. 2011 Jul 17-20; Abstract No. TUPE307.
- Whitmore SW, Taylor AW, Espinoza L, Shouse FL, Lampe MA, Nesheim SR. Correlates of mother-to-child HIV transmission in the United States and Puerto Rico. Pediatrics 2012 Jan;129:e74-81.
- Taylor AW, Nesheim S, Whitmore S, et al. Estimated number and characteristics associated with perinatal HIV infections, 33 states, United States, 2003–2007. 6th IAS Conference on HIV Pathogenesis, Treatment and Prevention (IAS 2011). Rome, Italy. 2011 Jul 17-20; Abstract No. TUPDC0103.
- CDC. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR 2006;55(RR-14):1-17
- Barrow RY, Newman LM, Douglas JM Jr. Taking positive steps to address STD disparities for African American communities. Sex Transm Dis 2008;35(12 Suppl):S1-S3.
- Gaur AH, Dominguez KL, Kalish ML, et al. Practice of feeding premasticated food to infants: a potential risk factor for HIV transmission. Pediatrics 2009;124:658-66.
- Lampe MA, Smith DK, Anderson GJ, Edwards AE, Nesheim SR. Achieving safe conception in HIV-discordant couples: the potential role of oral preexposure prophylaxis (PrEP) in the United States. Am J Obstet Gynecol 2011;204:488.e1-8.
- Luzuriaga K, Tabak B, Garber M, et al. HIV Type 1 (HIV-1) Proviral Reservoirs Decay Continuously Under Sustained Virologic Control in HIV-1–Infected Children Who Received Early Treatment J Infect Dis 2014; 210(10):1529-38.
Other Resources
Web Sites
National Women and Girls HIV/AIDS Awareness Day
AIDS Alliance for Children, Youth, & Families
Mother to Child Transmission Resources (AIDS Education and Training Centers)
HIV/AIDS (womenshealth.gov)
Women, Children, and HIV (University of California, San Francisco)
Cervical Cancer and HIV (SmartGlobalHealth.org)
Pregnancy and HIV, Viral Hepatitis, STD, and TB Prevention
General Resources
- CDC-INFO 1-800-CDC-INFO (232-4636)
- CDC HIV Website
- CDC Act Against AIDS Campaign
- CDC HIV Risk Reduction Tool (BETA)
- Page last reviewed: September 14, 2017
- Page last updated: September 14, 2017
- Content source: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention


 ShareCompartir
ShareCompartir