HIV Among Men in the United States
Fast Facts
- Men accounted for 76% of all adults and adolescents living with HIV infection at the end of 2010 in the United States.
- Men who have sex with men account for most new and existing HIV infections among men.
- By race/ethnicity, black men have the highest rates of new HIV infections among all men.
 In 2010, an estimated 1.1 million people aged 13 years or older were living with HIV infection in the United States. Most (76%) of those living with HIV were male, and 69% of males were gay, bisexual, and other men who have sex with men (MSM)a.
In 2010, an estimated 1.1 million people aged 13 years or older were living with HIV infection in the United States. Most (76%) of those living with HIV were male, and 69% of males were gay, bisexual, and other men who have sex with men (MSM)a.
In 2010, the most recent year for which new HIV infection data are available, men accounted for 80% (38,000) of the estimated 47,500 new HIV infections. Most infections occurred in adults aged 25 to 34 years, except among black/African American men (referred to as “black” in this fact sheet), for whom 38% of all new infections occurred in the youngest age group, 13 to 24 years.
The Numbers
New HIV Infectionsb in 2010
- There were an estimated 38,000 new HIV infections among men in the United States. Seventy-eight percent (29,800) of these were among MSM.
- Of the 38,000 total estimated new HIV infections in US men, 39% (14,700) were in blacks, 35% (13,200) were in whites, and 22% (8,500) were in Hispanics/Latinos.c
- The rate of estimated new HIV infections among black men (per 100,000) was 103.6—six and a half times that of white men (15.8) and more than twice the rate among Hispanic/Latino men (45.5).
Estimated Numbers of New HIV Infections in the United States for the Most Affected Subpopulations, 2010
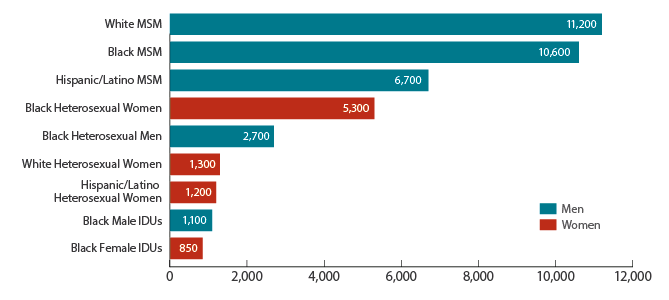
Source: CDC. Estimated HIV incidence among adults and adolescents in the United States, 2007–2010. HIV Surveillance Supplemental Report 2012;17(4). Subpopulations representing 2% or less of the overall US epidemic are not reflected in this chart.
Abbreviations: IDU, injection drug user; MSM, men who have sex with men.
HIV and AIDS Diagnoses and Deaths
- The Centers for Disease Control and Prevention (CDC) estimates that 1 in 51 men will receive a diagnosis of HIV infection at some point in their lifetimes. Over the course of their lifetimes, 1 in 16 black men will be diagnosed with HIV infection, as will 1 in 33 Native Hawaiian/Other Pacific Islander men, 1 in 36 Hispanic/ Latino men, 1 in 100 American Indian/Alaska Native men, 1 in 102 white men, and 1 in 145 Asian men.
- Overall, an estimated 16% of all adults and adolescents living with HIV infection in 2010 were undiagnosed. Among men, greater percentages of undiagnosed HIV infections were attributed to male-to-male sexual contact (19%) and heterosexual contact (19%)e compared to other transmission categories.
- In 2011, 79% (38,825) of the 49,273 estimated new diagnoses of HIV infection (including children) in the United States were among adult and adolescent men. Black/African American men (referred to as “black” in this fact sheet) had the highest rate of HIV diagnosis among all races/ethnicities.
- In 2011, 75% (24,088) of the 32,052 estimated AIDS diagnoses in the United States (including children) were among men. Men represent 79% (913,368) of the estimated 1,155,792 people (including children) diagnosed with AIDS in the United States through the end of 2011.
- In 2010, 74% (11,515) of the estimated 15,529 people with a diagnosis of AIDS who died in the United States (regardless of cause of death) were men.
- From 2000 to 2010, HIV infection was the 7th leading cause of death overall for black men, but was not a leading cause of death for other races/ethnicities.
Prevention Challenges
Like other populations affected by HIV, men face a number of risk factors that contribute to their risk for HIV infection.
Sexual contact: Most HIV infections in men are transmitted through sexual contact, especially anal sex.
Sexually transmitted infections (STIs): The presence of some STIs greatly increases the likelihood of acquiring or transmitting HIV. Rates of gonorrhea and syphilis are higher among black men than among white or Hispanic/Latino men. Rates of syphilis have increased in recent years among MSM.
Injection drug and other substance use: The use of injection drugs or other substances may increase the risk of HIV infection through sharing injection equipment contaminated with HIV or engaging in high-risk behaviors, such as unprotected sex, when under the influence of drugs or alcohol.
What CDC Is Doing
Guided by the National HIV/AIDS Strategy for the United States, CDC and its partners are pursuing a High-Impact Prevention approach to reducing new HIV infections by using combinations of scientifically proven, cost-effective, and scalable interventions directed to the most vulnerable populations in the geographic areas where HIV prevalence is highest. For example,
The MSM Testing Initiative aims to identify at least 3,000 HIV-infected MSM who were previously unaware of their infection, at least half of whom may be Hispanic/Latino or black, and link at least 2,550 (85%) of these HIV-infected MSM to HIV medical care.
CDC recently awarded $55 million over 5 years to 34 community-based organizations to provide HIV testing to more than 90,000 young gay and bisexual men and transgender youth of color, with a goal of identifying more than 3,500 previously unrecognized HIV infections and linking those who are HIV-infected to care and prevention services.
The agency supports research to develop new interventions and to adapt existing interventions for populations at increased risk for HIV infection and those living with HIV infection. CDC also supports the national dissemination of effective HIV behavioral interventions for men. Mpowerment, for example, encourages young gay and bisexual men of diverse backgrounds to reduce sexual risk taking, get regular HIV testing, and build positive social connections.
Through the National HIV Behavioral Surveillance System, CDC collects data on behavioral risks, testing behaviors, access to and use of prevention services, and testing results on MSM and high-risk heterosexual men to better understand the drivers of HIV infection.
Act Against AIDS campaigns and other collaborative activities provide men with effective and culturally appropriate messages about HIV prevention. The Reasons/ Razones testing campaign features Hispanic/Latino gay and bisexual men sharing their reasons for getting an HIV test, while Testing Makes Us Stronger encourages black gay and bisexual men to get tested for HIV.Let’s Stop HIV Together focuses on raising awareness of HIV and AIDS and simultaneously combating complacency and stigma by increasing support for people living with the disease.
CDC has issued interim guidance on pre-exposure prophylaxis for providers for use with their patients at highest risk for becoming infected with HIV.
aThe term men who have sex with men (MSM) is used in CDC surveillance systems. It indicates a behavior that transmits HIV infection, not how individuals self-identify in terms of their sexuality.
bNew HIV infections refers to HIV incidence, or the number of people who are newly infected with HIV within a given period of time, whether they are aware of their infection or not.
c Hispanics/Latinos can be of any race.
Bibliography
- CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 U.S. dependent areas—2011. HIV Surveillance Supplemental Report 2013;18(5).
- Centers for Disease Control and Prevention. Estimated HIV incidence among adults and adolescents in the United States, 2007–2010. HIV Surveillance Supplemental Report 2012;17(4).
- CDC. Diagnoses of HIV infection and AIDS in the United States and dependent areas, 2011. HIV Surveillance Report 2013;23.
- CDC. Estimated lifetime risk for diagnosis of HIV infection among Hispanics/Latinos – 37 states and Puerto Rico, 2007. MMWR 2010;59(40):1297-1301.
- CDC. WISQARS leading causes of death reports, national and regional, 1999–2010. Accessed May 13, 2013.
- CDC. 2011 National data for chlamydia, gonorrhea, and syphilis.
Additional Resources
- CDC-INFO 1-800-CDC-INFO (232-4636)
- CDC HIV Website
- CDC Act Against AIDS Campaign
- CDC HIV Risk Reduction Tool (BETA)
- Page last reviewed: March 9, 2017
- Page last updated: March 9, 2017
- Content source: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention


 ShareCompartir
ShareCompartir