About 1 in 10 U.S. pregnant women with confirmed Zika infection had a fetus or baby with birth defects in 2016
Press Release
Embargoed Until: Tuesday, April 4, 2017; 1:00 p.m. ET
Contact: Media Relations
(404) 639-3286
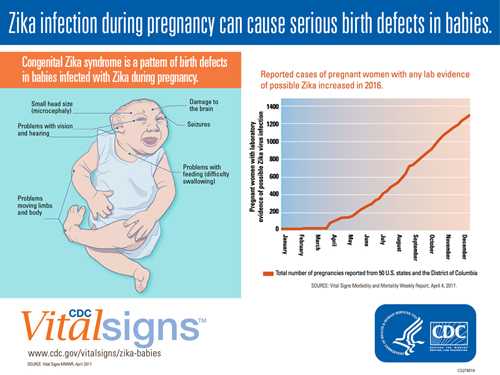
Zika infection during pregnancies can cause serious birth defects in babies. Entire Infographic
Of the 250 pregnant women who had confirmed Zika infection in 2016, 24 – or about 1 in 10 of them – had a fetus or baby with Zika-related birth defects, according to a new Vital Signs report from the Centers for Disease Control and Prevention (CDC). This report is the first to provide the analysis of a subgroup of pregnant women in the U.S. with clear, confirmed test results of Zika virus infection.
Testing for Zika remains complex because there is a narrow timeframe for obtaining a positive laboratory result, and many infected people do not have symptoms that might motivate testing. For this reason, CDC is monitoring all pregnant women with any evidence of recent Zika infection. In 2016, nearly 1,000 pregnant women from 44 states who completed their pregnancies had some evidence of a recent Zika infection and were at risk of having a fetus or baby with Zika-related birth defects. Most of these women acquired Zika infection during travel to an area where Zika was known to be present.
Zika infection during pregnancy can cause serious damage to the brain and microcephaly in developing fetuses. It also can lead to congenital Zika syndrome in babies, a pattern of birth defects that includes brain abnormalities, vision problems, hearing loss, and problems moving limbs. Babies may also appear healthy at birth but have underlying brain defects or other Zika-related health problems.
“Zika virus can be scary and potentially devastating to families. Zika continues to be a threat to pregnant women across the U.S.,” said CDC Acting Director Anne Schuchat, M.D. “With warm weather and a new mosquito season approaching, prevention is crucial to protect the health of mothers and babies. Healthcare providers can play a key role in prevention efforts.”
In 2016, pregnant women with evidence of Zika were reported in 44 states. Most became infected through travel to an area with Zika.
The findings from this report confirm the serious threat posed by Zika virus infection during pregnancy and the critical need for pregnant women to continue taking steps to prevent Zika virus exposure through mosquito bites and sexual transmission. The report also emphasizes the importance of healthcare providers screening all pregnant omen for possible Zika virus exposure and testing and evaluating all infants born to women with evidence of Zika infection.
Identifying scope of Zika cases in U.S. and gaps in evaluation and care management
This report updates previously published estimates of the proportion of fetuses or babies with birth defects among pregnant women with possible Zika infection reported to the U.S. Zika Pregnancy Registry from January 15 to December 27, 2016 in the 50 U.S. states and Washington D.C. The Registry includes data from all U.S. states, DC, and all U.S. territories except Puerto Rico; pregnancies in Puerto Rico are monitored separately by the Zika Active Pregnancy Surveillance System. This report also highlights possible gaps in clinical evaluation and management of infants with possible congenital Zika virus infection.

Healthcare providers can stay up to date on CDC's Zika testing and follow-up guidance to give pregnant women and affected babies the best care possible.
Key findings in the Vital Signs report include:
- Forty-four states reported pregnant women with evidence of Zika in 2016.
- Most of these women acquired Zika virus infection during travel to an area with Zika.
- Nearly 1,300 pregnant women with evidence of possible Zika infection were reported to the U.S. Zika Pregnancy Registry.
- Of the 1,000 pregnancies that were completed by the end of the year, more than 50 had Zika-related birth defects.
- Among pregnant women with confirmed Zika infection, about 1 in 10 had a fetus or baby with birth defects.
- Confirmed infections in the first trimester posed the highest risk – with about 15% having Zika-related birth defects.
- About 1 in 3 babies with possible congenital Zika infection had no report of Zika testing at birth.
- Only 1 in 4 babies with possible congenital Zika infection were reported to have received brain imaging after birth.
“CDC recommends that pregnant women avoid travel to areas with risk of Zika and unprotected sex with a partner who has traveled to an area with Zika to prevent Zika-related birth defects in their babies,” said Peggy Honein, Ph.D., the Zika Response’s Pregnancy and Birth Defects Task Force co-lead. “CDC continues to work closely with health departments on the U.S. Zika Pregnancy Registry to follow up infants with possible congenital Zika virus infection and better understand the full range of disabilities that can result from this infection.”
CDC encourages healthcare providers to:
- Educate families on Zika prevention.
- Provide all needed tests and follow-up care.
- Support babies and families.
CDC is continuously updating guidance for healthcare providers on testing and clinical care for pregnant women and babies affected by Zika. It is also monitoring new infections and working to identify the long-term outcomes of congenital Zika infection.
To learn more about Zika virus, visit https://www.cdc.gov/zika/. Healthcare providers can visit https://www.cdc.gov/zika/hc-providers/index.html for CDC’s latest clinical guidance, testing, and training information for Zika.
About Vital Signs
Vital Signs is a report that appears as part of the CDC’s Morbidity and Mortality Weekly Report. Vital Signs provides the latest data and information on key health indicators: cancer prevention, obesity, tobacco use, motor vehicle passenger safety, prescription drug overdose, HIV/AIDS, alcohol use, health care-associated infections, cardiovascular health, teen pregnancy, food safety, and viral hepatitis.
- Page last reviewed: April 6, 2017
- Page last updated: April 6, 2017
- Content source:


 ShareCompartir
ShareCompartir