We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Acute angle-closure glaucoma
From WikEM
Contents
Background
Pathophysiology
- Obstructed aqueous outflow tract → aqueous humor builds up → increased intraocular pressure (IOP) → optic nerve damage → vision loss
- Increased posterior chamber pressure causes iris to bulge forward (iris bombé) → further obstruction of outflow tract → further increase IOP
- Acute attack is usually precipitated by pupillary dilation
Clinical Features
- Abrupt onset of severe (usually unilateral) eye pain
- Blurred vision
- Frontal or supraorbital headache
- Nausea / vomiting / abdominal pain
Differential Diagnosis
Unilateral Red Eye
- Acute angle-closure glaucoma^
- Anterior uveitis
- Caustic keratoconjunctivitis^^
- Conjunctival laceration
- Conjunctivitis
- Corneal abrasion
- Corneal erosion
- Ocular foreign body
- Corneal ulcer^
- Endophthalmitis^
- Episcleritis
- Globe rupture^
- Herpes zoster ophthalmicus
- Intraocular foreign body
- Inflamed pingueculum
- Inflamed Pterygium
- Keratoconjunctivitis
- Keratoconus
- Lens dislocation
- Nontraumatic iritis
- Scleritis^
- Subconjunctival hemorrhage
- Traumatic hyphema
- Traumatic iritis
- Ultraviolet keratitis
^Emergent diagnoses
^^Critical diagnoses
Evaluation
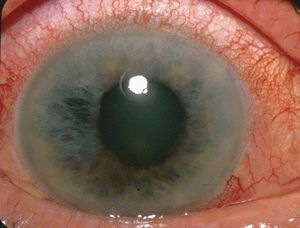
- Fixed, midposition pupil
- Hazy cornea
- Conjunctival injection most prominent at limbus (ciliary flush)
- Rock-hard globe
- IOP >20 mm Hg
- Slit lamp exam shows shallow anterior chamber and cell and flare
Definition: 3 signs + 2 symptoms
- At least 3 of these signs:
- IOP >21 mm Hg
- Conjunctival injection
- Corneal epithelial edema
- Mid-dilated nonreactive pupil
- Shallow anterior chamber with occlusion
- At least 2 of these symptoms:
- Ocular pain
- Nausea/vomiting
- History of intermittent blurring of vision with halos
Management
Goal of medical therapy is to 'break the attack' in order to prepare the patient for laser iridotomy.[1]
- Emergent ophthalmology consult
- Recheck IOP at least hourly
- Supine position to decrease IOP
- Place patient in a well lit room (prevent pupillary dilation)
- Start with a topical beta-blocker, alpha blocker and PO acetazolamide if no contraindications
Decrease production of aqueous humor
Timolol 0.5%:
- Blocks beta receptors on ciliary epithelium
- 1 drop in affected eye, repeat in 1 hour if needed.
- Blocks productions of HCO3-, which draws Na+ into the eye; water follows by osmosis to form aqueous humour
- 500mg IV or PO (PO preferred unless patient is nauseated)
- Can substitute methazolamide 100mg if patient has renal failure.
- Contraindicated in sickle cell patients
Dorzolamide (Trusopt) 2%:
- topical carbonic anhydrase inhibitor
- 1 drop in affected eye
Alpha agonist
Brimonidine ophthalmic (Alphagan) 0.2% OR Apraclonidine ophthalmic 1%:
- Alpha agonist will increase trabecular outflow
- 1 drop in affected eye
Facilitate outflow of aqueous humor
Pilocarpine 1%–2%:
- Parasympatholytic alkaloid acts on muscarinic receptors found on iris sphincter muscle → causes muscle to contract → miosis → pulls iris away from trabecular network
- 1 drop in affected eye every 15 minutes x 2-4 doses, then every 4 to 6 hours
- Likely does not work until IOP drops below 40-50 mmHg, but still give immediately upon diagnosis
- Note: may make fundoscopic evaluation more difficult for ophtho consultant due to miosis
Reduce volume of aqueous humor
These therapies are usually resolved for failure of other treatments. Hyper osmotic agents such as mannitol are effective but are contraindicated in renal failure and can cause hypotension in the volume depleted patient.
- Mannitol: 1-2 g/kg IV (most common)
- 50% glycerin (Osmoglyn) OR 45% isosorbide (Ismotic): 1.5 mL/kg PO (rarely used)
Steriods
Topical steroids not indicated during acute attack, but may help inflammation after IOP under control.
See Also
References
- ↑ Primary Angle Closure Preferred Practice Pattern Guideline. American Academy of Ophthalmology. Angle Closure PPP Accessed 06/17/15.