We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Corneal abrasion
From WikEM
(Redirected from Corneal Abrasion and Foreign Body)
Contents
Background
- Must rule-out intraocular foreign body and corneal laceration
Clinical Features
- Foreign body sensation
- Photophobia (+/- consensual)
- Decreased vision
- If associated iritis or if abrasion occurs in visual axis
- Relief of pain with topical anesthesia
- Virtually diagnostic of corneal abrasion
Differential Diagnosis
Unilateral Red Eye
- Acute angle-closure glaucoma^
- Anterior uveitis
- Caustic keratoconjunctivitis^^
- Conjunctival laceration
- Conjunctivitis
- Corneal abrasion
- Corneal erosion
- Ocular foreign body
- Corneal ulcer^
- Endophthalmitis^
- Episcleritis
- Globe rupture^
- Herpes zoster ophthalmicus
- Intraocular foreign body
- Inflamed pingueculum
- Inflamed Pterygium
- Keratoconjunctivitis
- Keratoconus
- Lens dislocation
- Nontraumatic iritis
- Scleritis^
- Subconjunctival hemorrhage
- Traumatic hyphema
- Traumatic iritis
- Ultraviolet keratitis
^Emergent diagnoses
^^Critical diagnoses
Evaluation
- A complete eye exam should be conducted
- Eyelid Exam
- Flip upper lid and exam lower lid for FB
- If concern for FB despite normal exam, consider orbital CT or MRI is certain it is nonmetallic
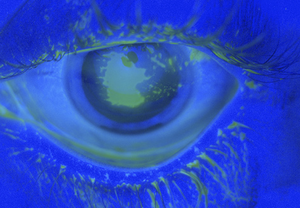
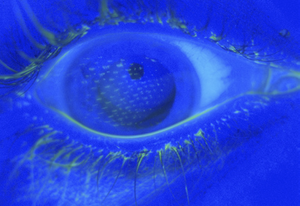
- Fluorescein Exam
- Apply 1 gtt of flourescein or utilize strip with anesthetic
- Use Wood's Lamp or Slit Lamp with colbalt blue light
- Fluoresceine will fill corneal defects and glow
- Multiple vertical abrasions suggests foreign body embedded under the upper lid
Additional Considerations
- Contact lens wearer
- If white spot or opacity on exam concerning for infiltrate or ulceration refer for same day ophtho appt
- Fluorescein Examination
- Seidel sign (streaming of fluorescein) indicates penetrating trauma
- Branching/Dendritic pattern suggests possible Herpes Zoster Ophthalmicus
- Visual acuity
- If poor, consider corneal edema versus infectious infiltrate
- Pupil shape and reactivity
- Irregular or nonreactive pupil suggests pupillary sphincter injury and possible penetrating trauma
- Hyphema or hypopyon
- Hyphema suggests possible penetrating injury
- If present then same same-day ophtho consult is required
- Extruded ocular contents
- If yes then place eye shield and obtain emergent ophtho referral
- Corneal Ulcer
- Grayish white lesion
- Worsening symptoms >1day
Management
Antibiotics
Does Not Wear Contact Lens
- Erythromycin ointment qid x 3-5d OR
- Ciprofloxacin 0.3% ophthalmic solution 2 drops q6 hours
- Ofloxacin 0.3% solution 2 drops q6 hours
- Sulfacetamide 10% ophthalmic ointment q6 hours
Wears Contact Lens
Antibiotics should cover pseudomonas and favor 3rd or 4th generation fluoroquinolones
- Levofloxacin 0.5% solution 2 drops ever 2 hours for 2 days THEN q6hrs for 5 days OR
- Moxifloxacin 0.5% solution 2 drops every 2 hours for 2 days THEN q6hrs for 5 days OR
- Tobramycin 0.3% solution 2 drops q6hrs for 5 days OR
- Gatifloxacin 0.5% solution 2 drops every 2 hours for 2 days THEN q6hrs for 5 days OR
- Gentamicin 0.3% solution 2 drops six times for 5 days
Analgesia
- Systemic NSAIDs or opioids
- Cycloplegics can be consider for patients with large abrasions (>2mm) and/or severe pain
- Cyclopentolate 1% 1 drop q6-8hr
- Ophthalmic NSAIDs
- Ketorolac 0.4% 1 drop q6hr x 2-3d
- Topical anesthetics
- Tetracaine 1% 1 drop q30min has been found to be safe in the first 24 hrs[1]
Other
- Tetanus prophylaxis not indicated (unless penetrating injury)[2]
- Patch is not routinely recommended[3] and can prolong healing time[4]
Disposition
- Ophtho follow up in 48h for routine cases
- Minor abrasions will heal in 48h
References
- ↑ Waldman N, et al. Topical tetracaine used for 24 hours is safe and rated highly effective by patients for the treatment of pain caused by corneal abrasions: a double-blind, randomized clinical trial. Acad Emerg Med. 2014; 21(4):374-82.
- ↑ Mukherjee P, et al. Tetanus prophylaxis in superficial corneal abrasions. Emerg Med J. 2003; 20:62-64.
- ↑ Flynn CA, et al. Should we patch corneal abrasions? A meta-analysis. J Fam Pract. 1998; 47(4):264-70.
- ↑ Fraser, S. Corneal abrasion. Clin Ophthalmol. 2010; 4:387-390.