We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
EBQ:Denver Screening Criteria
From WikEM
Contents
Background
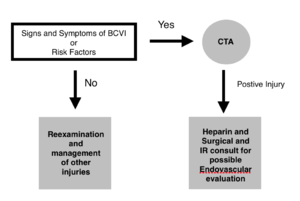
- Used to screen for vertebral and carotid artery dissection and/or injury after blunt head and neck trauma (BCVI - blunt cerebrovascular injury)[1][2]
- A CTA to evaluate for VAI should be obtained in those meeting the modified Denver Criteria
- BCVI has the highest association with cervical hyperextension and rotation, hyperflexion, or direct blunt force to head and neck[3]
- Most injuries are diagnosed after the development of symptoms secondary to central nervous system ischemia resulting in neurologic morbidity of up to 80% and associated mortality of up to 40%.[4]
Clinical Question
- Can clinical criteria and injury profile and risk factors successfully identify patients at risk for BCVI?
Conclusion
Denver criteria can successfully identify trauma patients at risk for vascular injury.
- 5% of trauma patients were screened
- 18% of screened patients had a vascular injury
The Denver Screening Criteria are divided into risk factors and signs and symptoms
Signs and Symptoms
- Focal neurologic deficit
- Arterial Hemorrhage
- Cervical Bruit or Thrill (<50yo)
- Infarct on Head CT
- Expanding Neck Hematoma
- Neuro exam inconsistent with Head CT
Risk Factors
- Midface Fractures
- Cervical Spine Injuries
- Basilar Skull Fracture
- GCS<8
- Hanging with Anoxic Brain Injury
- Seat belt abrasion or other soft tissue injury of the anterior neck resulting in significant swelling or altered mental status
- Kerwin et al: Using the above criteria for both symptomatic and asymptomatic patients, found a 44% positive angiography rate in 1941 patients.[7]
- Fabian et al: Reported a drop in BCI-associated mortality from 24% to 13% after instituting a broad screening protocol.[8]
Validation
- The Denver Criteria has not been externally validated
- The Memphis Criteria which includes many of the same criteria screened 3.9% of patients and found an incidence of 29% vascular injury in screened patients.
- Cervical Spine Fracture
- Neuro deficit not explained by brain imaging
- Horner's Syndrome
- Leforte 2 or 3 fracture
- Basilar Skull Fracture involving the carotid Canal
- Seatbelt Sign
- Neck Hematoma
- Hanging Mechanism
See Also
Sources
- ↑ Bromberg, William. et al. Blunt Cerebrovascular Injury Practice Management Guidelines: The Eastern Association for the Surgery of Trauma. J Trauma. 68 (2): 471-7, Feb 2010.
- ↑ Cothren CC, Moore EE, Biffl WL, et al. Anticoagulation is the gold standard therapy for blunt carotid injuries to reduce stroke rate. Arch Surg. 2004;139:540–545; discussion 545–546. PDF
- ↑ Biffl WL, Moore EE, Offner PJ, et al. Optimizing screening for blunt cerebrovascular injuries. Am J Surg. 1999;178:517–522.
- ↑ Davis JW, Holbrook TL, Hoyt DB, Mackersie RC, Field TO Jr, Shackford SR. Blunt carotid artery dissection: incidence, associated injuries, screening, and treatment. J Trauma. 1990;30:1514–1517
- ↑ DiPerna CA, Rowe VL, Terramani TT, et al. Clinical importance of the “seat belt sign” in blunt trauma to the neck. Am Surg. 2002;68:441–445
- ↑ Rozycki GS, Tremblay L, Feliciano DV, et al. A prospective study for the detection of vascular injury in adult and pediatric patients with cervicothoracic seat belt signs. J Trauma. 2002;52:618–623; discussion 623–624
- ↑ Kerwin AJ, Bynoe RP, Murray J et al. Liberalized screening for blunt carotid and vertebral artery injuries is justified. J. Trauma 2001; 51: 308–14.
- ↑ Fabian TC, Patton JH, Croce MA et al. Blunt carotid injury: importance of early diagnosis and anticoagulant therapy. Ann. Surg.1996; 223: 513–25.