We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
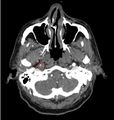
Vertebral and carotid artery dissection
From WikEM
Contents
Background
- Most frequent cause of CVA in young and middle-aged patients (median age - 40yrs)
- Symptoms may be transient or persistent
- Consider in trauma patient who has neurologic deficits despite normal head CT
- Consider in patient with CVA + neck pain
Risk Factors
- Neck trauma (often minor)
- Cervical manipulation
- Coughing
- Connective tissue disease
- History of migraine[1]
Clinical Features
Internal Carotid Dissection
- Unilateral headache, face pain, anterior neck pain
- Pain can precede other symptoms by hours-days (median 4d)
- Headache most commonly is frontotemporal; severity may mimic SAH or preexisting migraine
- Partial Horner syndrome (miosis and ptosis) in 50% of cases
- Cranial nerve palsies
Vertebral Artery Dissection
- Posterior neck pain, headache
- May be unilateral or bilateral
- Headache is typically occipital
- Unilateral facial paresthesia
- Dizziness
- Vertigo
- Nausea/vomiting
- Diplopia and other visual disturbances
- Ataxia
- Lateral Medullary Syndrome seen in up to 20% of cases of VAD[2][3]
Differential Diagnosis
Blunt Neck Trauma
- Spinal cord trauma
- Vertebral and carotid artery dissection
- Whiplash injury
- Cervical spine fractures and dislocations
- Strangulation
Evaluation
The Denver Screening Criteria are divided into risk factors and signs and symptoms
Signs and Symptoms
- Focal neurologic deficit
- Arterial Hemorrhage
- Cervical Bruit or Thrill (<50yo)
- Infarct on Head CT
- Expanding Neck Hematoma
- Neuro exam inconsistent with Head CT
Risk Factors
- Midface Fractures
- Cervical Spine Injuries
- Basilar Skull Fracture
- GCS<8
- Hanging with Anoxic Brain Injury
- Seat belt abrasion or other soft tissue injury of the anterior neck resulting in significant swelling or altered mental status
If Denver Criteria positive, CTA or MRA
- CTA has been shows to be equivalent to MRA
Management
Anti-coagulation followed by vascular repair is the generally accepted treatment. Anti-coagulation prevents clot propagation along the dissecting lumen[6]
tPA
- Do not give if dissection enters the skull (ie Intracranial)
- Do not give if aorta is involved
- Otherwise, give according to same guidelines as for ischemic CVA (see CVA (tPA))
Antiplatelet vs Anticoagulation Therapy
Very controversial with poor data
- Heparin: If dissection causes neuro deficits and is EXTRACRANIAL
- Aspirin: If dissection is INTRACRANIAL
- Aspirin: If dissection is extracranial but no neuro deficit, for prevention of thrombo-embolic event
- If tPA was given, wait 24hr before starting antiplatelet therapy
- Do not give if NIHSS score ≥ 15 (risk of hemorrhagic transformation)
Endovascular Therapy
- Emergent consultation with vascular surgery.
- tPA use does not exclude patients from endovascular therapy
Complications
- CVA
- Risk of stroke or recurrent stroke is highest in the first 24hr after dissection
- SAH (if dissection extends intracranially)
See Also
References
- ↑ De Giuli V et al. Association Between Migraine and Cervical Artery Dissection: The Italian Project on Stroke in Young Adults. JAMA Neurol. Published online March 6, 2017. doi:10.1001/jamaneurol.2016.5704
- ↑ Lee MJ, Park YG, Kim SJ, Lee JJ, Bang OY, Kim JS. Characteristics of stroke mechanisms in patients with medullary infarction. Eur J Neurol. 2012;19(11):1433-1439.
- ↑ Kim JS. Pure lateral medullary infarction: clinical-radiological correlation of 130 acute, consecutive patients. Brain. 2003;126(Pt 8):1864-1872.
- ↑ DiPerna CA, Rowe VL, Terramani TT, et al. Clinical importance of the “seat belt sign” in blunt trauma to the neck. Am Surg. 2002;68:441–445
- ↑ Rozycki GS, Tremblay L, Feliciano DV, et al. A prospective study for the detection of vascular injury in adult and pediatric patients with cervicothoracic seat belt signs. J Trauma. 2002;52:618–623; discussion 623–624
- ↑ Zinkstok SM, Vergouwen MD, Engelter ST, et al. Safety and functional outcome of thrombolysis in dissection-related ischemic stroke: a meta-analysis of individual patient data. Stroke. 2011;42:2515–2520.