We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Focal neurologic deficits
From WikEM
(Redirected from Focal neurologic signs)
Contents
Background
- Also known as focal neurologic signs
- Refer to objective abnormalities of a specific region of the body detected on the neurologic examination
Focal Neurologic Signs Organized by Region
Brain
- Frontal Lobe
- Damage to the frontal lobe can lead to the following signs:
- Sensorimotor deficit of the contralateral lower extremity
- Language disturbances
- Profound behavioral changes
- Indifference, apathy
- Disinhibition (labile and irritable)
- Impaired judgement, decreased social graces
- Akinesia (lack of spontaneous movements)
- Impairment of memory
- Damage to the frontal lobe can lead to the following signs:
- Parietal Lobe
- Damage to the parietal lobe can lead to the following signs:
- Agnosia
- Anosognosia – Unawareness of a deficit
- Unilateral spatial neglect (hemineglect)
- Dyslexia, dysgraphia, dyscalculia
- Impairment of tactile sensation
- Damage to the parietal lobe can lead to the following signs:
- Temporal Lobe
- Damage to the temporal lobe can lead to the following signs:
- Upper homonymous quadrantanopsia
- Cortical deafness
- Wernicke’s aphasia (word deafness, auditory verbal agnosia)
- Hallucinations
- Complex partial seizures
- Kluver-Bucy syndrome (Bilateral disease. Compulsion to attend all visual stimuli, hyperorality, hypersexuality, blunted emotional reactivity)
- Damage to the temporal lobe can lead to the following signs:
- Occipital Lobe
- Damage to the temporal lobe can lead to the following signs:
- Contralateral homonymous hemianopia
- Cortical blindness (bilateral lesions)
- Visual hallucinations
- Prosopagnosia
- Alexia without agraphia
- Loss of topographic memory and visual orientation
- Damage to the temporal lobe can lead to the following signs:
- Limbic System
- Damage to the limbic system can lead to the following signs:
- Retrograde amnesia (long-term memory loss)
- Anterograde amnesia (inability to form new memories)
- Apathy
- Loss of olfactory functions
- Cerebellar
- Damage to the cerebellum can lead to the following signs:
- Ataxia of voluntary movements
- Intention tremor
- Dysarthria
- Postural abnormalities
- Hypotonia
- Incoordination
- Nystagmus, gaze paresis
- Damage to the limbic system can lead to the following signs:
- Brainstem
- Damage to the brainstem can lead to the following signs:
- Crossed deficits – motor or sensory involvement of the face on one side of the body and the arm and leg on the other side
- Cranial nerve palsies (see below)
- Damage to the brainstem can lead to the following signs:
Cranial nerves
- CN I (Olfactory)
- Anosmia + perceived change in taste of food
- Deficit caused by shearing of the nerve ending passing through the cribriform plate usually by closed head trauma
- CN II (Optic)
- Monocular and binocular visual field defects
- Monocular: Giant cell arteritis, Anterior ischemic optic neuropathy, glaucoma, optic neuritis, trauma, increased ICP, emboli/arteritis/stenosis leading to retinal ischemia, ophthalmic artery or vein occlusion
- Binocular - Hemianopsia due to bilateral optic nerve disease.
- CN III (Oculomotor) –See Third Nerve Palsy
- CN IV (Trochlear)- See Trochlear nerve palsy
- CN VI (Abducens)- See Abducens nerve palsy
- Internuclear ophthalmoplegia - Lesion in medial longitudinal fasciculus, cannot adduct in horizontal lateral gaze, but normal convergence. Caused by multiple sclerosis or stroke
- CN V (Trigeminal)
- Jaw weakness and spasm. Jaw closure may be weak and/or asymmetric. +/- Trismus if irritative lesion to motor root.
- See trigeminal neuralgia
- CN VII (Facial)
- Upper motor neuron deficit – See Stroke, Hemorrhagic stroke, Multiple sclerosis, Amyotrophic Lateral Sclerosis (Upper and lower motor neuron disease)
- Sudden-onset of weakness: forehead sparing, facial droop
- Lower motor neuron deficit – See Bell's palsy
- Ipsilateral to defect: Inability to raise eyebrows, drooping of angle of mouth, incomplete closure of eyelid. No forehead sparing.
- Upper motor neuron deficit – See Stroke, Hemorrhagic stroke, Multiple sclerosis, Amyotrophic Lateral Sclerosis (Upper and lower motor neuron disease)
- CN VIII (Vestibular)
- Dysfunction may be characterized by: tinnitus, deafness, nausea, vertigo, balance issues
- See vertigo
- CN IX (Glossopharyngeal)
- Dysfunction may be characterized by: dysarthria, dysphagia
- CN X (Vagus)
- Dysfunction may be characterized by: hoarseness (unilateral vocal cord paralysis), dyspnea and inspiratory stridor (bilateral). Dysarthria, dysphagia.
- CN XI (Accessory)
- Dysfunction may be characterized by: Sternocleidomastoid and trapezius weakness leads to weak head rotation and shoulder shrug
- CN XII (Hypoglossal)
- Dysfunction may be characterized by: tongue deviation and wasting
Spinal Cord Syndromes
- Complete spinal cord transection syndrome
- Anterior cord syndrome
- Central cord syndrome
- Brown-Sequard syndrome
- Epidural compression syndromes
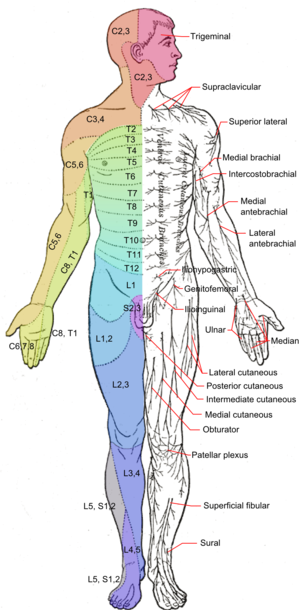
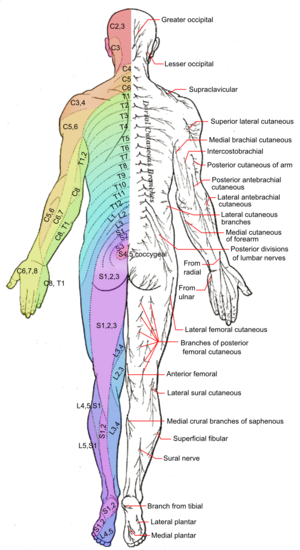
Peripheral nerve syndromes
- Upper extremity
- Ulnar
- Cause of Injury: Elbow injury.
- Sensory changes in the 5th and medial half of 4th digits, weak wrist flexors, “claw hand”
- Radial
- Cause of Injury: Distal humeral shaft fracture, anterior shoulder dislocation, supra-condylar fracture, Radial neuropathy at the spiral groove, Posterior interosseous neuropathy
- “Wrist drop,” weakness of finger extensors. +/- sensory loss over the dorsum of the hand, weak thumb adduction
- Median, distal
- Cause of Injury: Wrist dislocation, laceration, Carpal Tunnel Syndrome
- Weak flexion of radial half of digits and thumb, loss of abduction and opposition of thumb. Ape hand deformity, benediction sign. Loss of sensation of lateral three and one-half digits and nail beds
- Median, proximal
- Cause of Injury: Supracondylar humeral fracture, Pronator teres syndrome, Anterior interosseous neuropathy, tight cast
- See Median, distal above, loss of forearm pronation, loss of radial half digits and thumb flexion
- Musculocutaneous
- Cause of Injury: Anterior shoulder dislocation, entrapment due to hypertrophy
- Elbow flexion and supination weakness, radial forearm sensory deficits
- Axillary
- Cause of Injury: Anterior shoulder dislocation, inferior shoulder dislocation, proximal humerus fracture
- Weak arm abduction (from 15 to 90 degrees), weak shoulder flexion, extension and rotation of shoulder, loss of sensation of upper lateral arm
- Ulnar
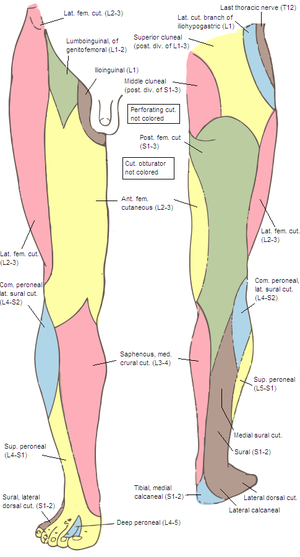
- Lower extremity
- Femoral
- Cause of Injury: Pubic rami fracture, pelvic fractures
- Weak knee extension, anterior knee sensory deficits
- Obturator
- Cause of Injury: Obturator ring fracture, obturator nerve entrapment
- Weak hip adduction, medial thigh sensory deficit
- Posterior tibial
- Cause of Injury: Knee dislocation
- Weak toe flexion, plantar foot sensory deficit
- Superficial peroneal
- Cause of Injury: Fibular neck fracture, knee dislocation
- Weak ankle eversion, lateral dorsal foot sensory deficits
- Deep peroneal
- Cause of Injury: Fibular neck fracture, compartment syndrome
- Sensory deficit at dorsal 1st web space, weak ankle and toe dorsiflexion
- Sciatic
- Cause of Injury: Posterior hip dislocation
- Lower leg weakness, foot drop, leg sensory deficits
- Superior gluteal
- Cause of Injury: Acetabular pelvic fracture
- Trendelenburg’s gait, Trendelenburg’s sign
- Inferior gluteal
- Cause of Injury: Acetabular pelvic fracture, s/p hip replacement
- Abnormal gait, gluteus maximus weakness resulting in gluteus maximus lurch
- Femoral
Evaluation
- Rule out acute causes of focal neurologic signs: stroke, hemorrhagic stroke, intracranial hemorrhage, meningitis
Management
- Treat underlying condition
Disposition
- Depending on cause
See Also
- Stroke
- Peripheral nerve syndromes
- Epidural compression syndromes
- Upper extremity peripheral innervation
References
- LeBlond RF, Brown DD, Suneja M, Szot JF. LeBlond R.F., Brown D.D., Suneja M, Szot J.F. LeBlond, Richard F., et al. DeGowin’s Diagnostic Examination, 10e. New York, NY: McGraw-Hill; 2015. http://accessmedicine.mhmedical.com.foyer.swmed.edu/content.aspx?bookid=1192&Sectionid=68670445. Accessed September 11, 2015.
- Waxman SG. Clinical Neuroanatomy, 27e. New York, NY: McGraw-Hill; 2013. http://accessmedicine.mhmedical.com.foyer.swmed.edu/content.aspx?bookid=673&Sectionid=45395961. Accessed September 07, 2015.
- Ropper AH, Samuels MA, Klein JP. Adams & Victor's Principles of Neurology, 10e. New York, NY: McGraw-Hill; 2014. http://accessmedicine.mhmedical.com.foyer.swmed.edu/content.aspx?bookid=690&Sectionid=50910870. Accessed September 07, 2015.
- Aminoff MJ, Greenberg DA, Simon RP. Disorders of Equilibrium. In: Aminoff MJ, Greenberg DA, Simon RP. eds. Clinical Neurology, 9e. New York, NY: McGraw-Hill; 2015. http://accessmedicine.mhmedical.com.foyer.swmed.edu/content.aspx?bookid=1194&Sectionid=68656660. Accessed September 08, 2015.
- Stone C, Humphries RL. eds. CURRENT Diagnosis & Treatment Emergency Medicine, 7e. New York, NY: McGraw-Hill; 2011. http://accessmedicine.mhmedical.com.foyer.swmed.edu/content.aspx?bookid=385&Sectionid=40357242. Accessed September 15, 2015.