We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Hypoglycemia
From WikEM
Contents
Background
- Brain depends on glucose as primary source of energy, but is unable to synthesize or store glucose
Common Anti-hyperglycemic Drugs and Pharmacology
| Drug | Pharmacology | ||
|---|---|---|---|
| Onset | Peak | Duration | |
Rapid-acting insulin
|
15-30min | 1-2h | 3-5h |
Short-acting insulin
|
30-60min | 2-4h | 6-10h |
Intermediate-acting insulin
|
1-3h | 4-12h | 18-24h |
Long-acting insulin
|
2-4h | None | 24h |
Sulfonylurea
|
– | 2-6h | 12-24h |
Clinical Features[1]
Neuroglycopenic
- Altered mental status, lethargy, confusion
- Focal neurologic deficits, visual disturbances
- Seizure
- Unresponsiveness
Autonomic
- Glucose levels < 55 mg/dL cause catecholamine surge[2]
- Anxiety, nervousness, irritability
- Nausea and vomiting
- Palpitations
- Tremor
- Changes in pupil size
- Tachycardia or bradycardia
- Salivation
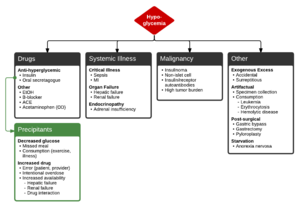
Differential Diagnosis
Hypoglycemia
Drugs
- Anti-hyperglycemic
- Insulin
- Oral secretagogue
- Other
Systemic Illness
- Critical Illness
- Organ Failure
- Hepatic failure
- Renal failure
- Endocrinopathy
- Seizure
Malignancy
- Insulinoma
- Non-islet cell
- Insulin/receptor autoantibodies
- High tumor burden
Other
- Artifactual
- Specimen collection
- Consumption
- Leukemia
- Erythrocytosis
- Hemolytic disease
- Post-surgical
- Gastric bypass
- Gastrectomy
- Pyloroplasty
- Starvation
Precipitants of anti-hyperglycemic induced hypoglycemia
- Decreased glucose
- Missed meal
- Consumption (exercise, illness)
- Increased drug
- Error (patient, provider)
- Intentional overdose
- Increased availability
- Hepatic failure
- Renal failure
- Drug interaction
Evaluation
Workup
- Patients with known diabetes who are not systemically ill and can identify a clear precipitant, no extensive workup is required.
- In severely ill patients, consider:
- BMP
- LFT
- EtOH
- Infectious workup: CXR, UA, urine and blood cultures
- ECG, troponin
- Other studies (not normally done in ED): insulin, C-peptide, pro-insulin, glucagon, growth hormone, cortisol, B-OH, insulin antibodies
- Exogenous insulin shows suppressed C-peptide levels (artificial insulin does not contain C-peptide)
- MEN-1 genetic testing for insulinoma suspicion[3]
- Elevated proinsulin and C-peptide during hypoglycemic episode in context of insulinoma
Evaluation[4]
"Whipple's Triad"
- Symptoms suggestive of hypoglycemia
- See Clinical Features
- Low glucose
- Serum glucose <60mg/dL
- Generally symptomatic at <55mg/dL though threshold is variable depending on chronicity
- Resolution of symptoms after administration of glucose
Management
- If altered mental status
- Dextrose 50% 50mL bolus (equals "one amp")
- Contains 25mg glucose
- Dextrose 50% 50mL bolus (equals "one amp")
- If awake
- Oral glucose
- Glucagon[5]
- Efficacy dependent on hepatic glycogen stores (less effective in chronic ETOH, cirrhosis, malnourished, neonate, in-born errors, glycogen storage disease, etc.)[6]
- Onset of action slower than IV dextrose (7-10min)
- 1mg SC or IM
Hypoglycemia from Sulfonylureas[7][8]
Activated charcoal[9]
- Administer activated charcoal, preferably within 1 hr of ingestion
- Multiple doses may be beneficial, especially for glipizide
Glucose Treatment
- Initial Therapy regardless of known cause
- Adults
- 50mL D50W bolus
- Start a D10 1/2NS drip (100mL/hr)
- Children
- 1mL/kg of D50W OR
- 2mL/kg D25W OR 5-10mL/kg D10W
- Neonate: 5-10 mL/kg D10W
Octreotide[10]
- Theoretical benefit to reduce risk of recurrent hypoglycemia
- Hyperpolarization of the beta cell results in inhibition of Ca influx and prevents insulin release
- 50-100 mcg subcutaneous in adults with repeat dosing Q6hrs
- 2 mcg/kg (max 150mcg) subcutaneously Q6hrs should be used in children
- Continuous infusion of 50-125 mcg/hr is an alternative in adults
- Administer octreotide for 24 hours, then after discontinuing, monitor for hypoglycemia for another 24 hours
Special Considerations
- Glucagon 5mg IM may be used as temporizing measure, e.g. while obtaining IV access
Hypoglycemia from Long Acting Insulin
- Similar treatment as for Sulfonylureas except no role for Octreotide
- Treatment should include oral intake as well as maintenance glucose containing drip either D5 or D10
Insulinoma[11]
- Symptomatic management as above
- Short acting octreotide, start at 50 μg SC TID, max 1500 μg per day
- SSTR2 and SSTR5 receptors at various levels on insulinomas, producing different response levels
- Octreotide can inhibit growth hormone and glucagon secretion, thereby worsening hypoglycemia in some pts[12]
- Long term medical management prior to surgery
- Diazoxide, start at 50 mg TID, max 400 mg per day, effective in ~50% of pts
- Long acting octreotide, 30 mg IM q28 days
Disposition
Admission or observation for oral anti-hyperglycemic agent or intermediate- to long-acting insulin. Consider discharge after 4h uneventful observation if:[13]
- Hypoglycemia fully and rapidly reversed without continuous infusion of dextrose
- Tolerated a full meal in ED
- Clear and innocuous cause identified with recurrence unlikely
- Adequate patient understanding, home support/monitoring, and ability to detect/prevent recurrence with close primary care follow-up
Insulinoma[14]
- Admission for 48-72 hrs of monitored fasting with q4 BGLs, insulin, C-peptide, proinsulin
- Then localization studies with US, CT, or MRI
See Also
References
- ↑ Jalili M. Type 2 Diabetes Mellitus In: Tintinalli's Emergency Medicine. 7th ed. McGraw Hill. 2011:1431-1432
- ↑ Grant CS. Insulinoma. Baillieres Clin Gastroenterol. 1996;10(4):645–671.
- ↑ O’Riordain DS, O’Brien T, van Heerden JA, Service FJ, Grant CS. Surgical management of insulinoma associated with multiple endocrine neoplasia type I. World J Surg. 1994;18(4):488–493; discussion 493–494.
- ↑ Jalili M. Type 2 Diabetes Mellitus In: Tintinalli's Emergency Medicine. 7th ed. McGraw Hill. 2011:1431-1432
- ↑ Carstens S, Sprehn M. Prehospital treatment of severe hypoglycaemia: a comparison of intramuscular glucagon and intravenous glucose. Prehosp Disaster Med. 1998 Apr-Dec;13(2-4):44-50
- ↑ Cydulka RK, Maloney GE. Diabetes Mellitus and Disorders of Glucose Homeostasis, in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2013, (Ch) 126: p 1652-1667.
- ↑ Rowden AK, Fasano CJ. Emergency management of oral hypoglycemic drug toxicity. Emerg Med Clin N Am 2007; 25:347-356
- ↑ Howland MA. Antidotes in Depth: Octreotide. In: Flomenbaum NE, Goldfrank LR, Hoffman RS et al, eds: Goldfrank’s Toxicologic Emergencies. New York NY, 2006;770-773
- ↑ Tran D et al. Oral Hypoglycemic Agent Toxicity Treatment & Management. Jul 14, 2015. http://emedicine.medscape.com/article/1010629-treatment#showall.
- ↑ Fasano CJ et al. Comparison of Octreotide and standard therapy versus standard therapy alone for the treatment of sulfonylurea-induced hypoglycemia. Ann Emerg Med 2008; 51:400-406
- ↑ Mathur A, Gorden P, Libutti SK. Insulinoma. Surg Clin North Am. 2009;89(5):1105–1121.
- ↑ Arnold R, Wied M, Behr TH. Somatostatin analogues in the treatment of endocrine tumors of the gastrointestinal tract. Expert Opin Pharmacother. 2002;3(6):643–656.
- ↑ Self, W. H., & McNaughton, C. D. (2013). Hypoglycemia. In Emergency Medicine (2nd ed., pp. 1379-1390). Elsevier.
- ↑ Taye A and Libutti SK. Diagnosis and management of insulinoma: current best practice and ongoing developments. Dove Press. 25 August 2015 Volume 2015:5 Pages 125—133.